Session Information
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Patients with autoimmune disease are at increased risk for complications from SARS-CoV-2 infection. We aimed to compare patient perspectives on COVID-19 vaccination among persons with and without autoimmune disease that were unvaccinated or who delayed receiving a COVID-19 vaccine.
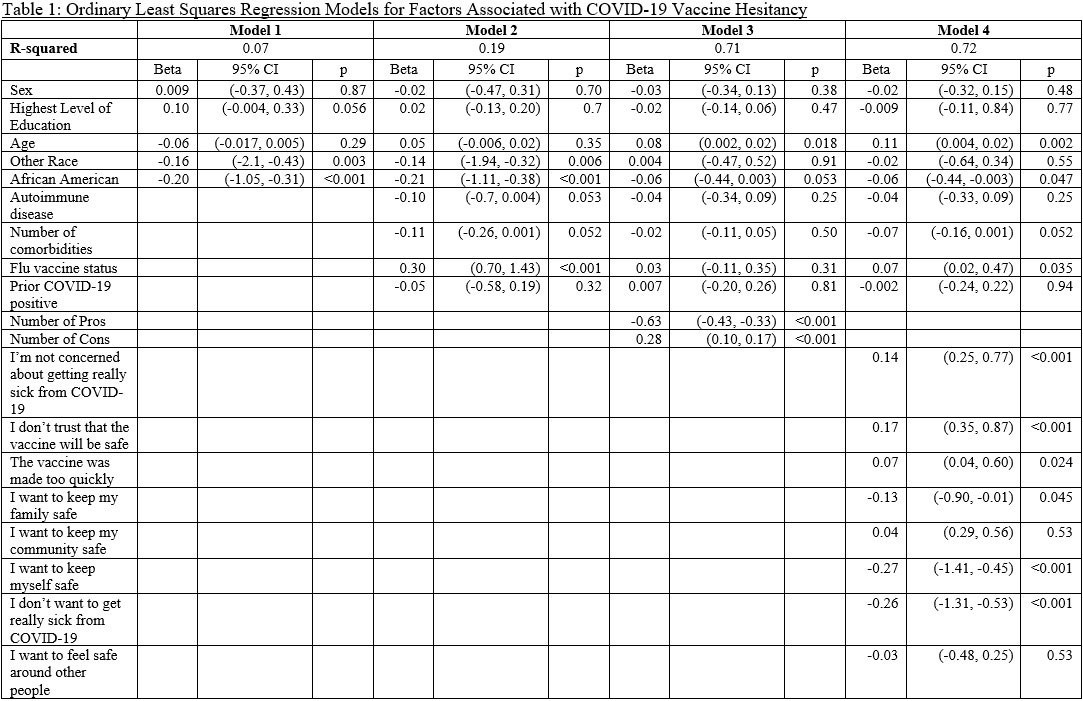
Methods: A 38-item questionnaire was given to 471 patients in rheumatology and primary care clinics at the MetroHealth System and Cleveland Veteran Affairs Medical Center between August 2021 and February 2022. The survey containing questions regarding demographics and perceptions of COVID-19 vaccines was administered to unvaccinated individuals and those who delayed vaccination for at least 2 months. Chi-square analyses were used to compare categorical variables. Multivariable ordinary least squares regression models were created to assess factors associated with COVID-19 vaccination likelihood. Regression analyses were reported as standardized coefficients and confidence intervals. All analyses were performed in SPSS version 28.
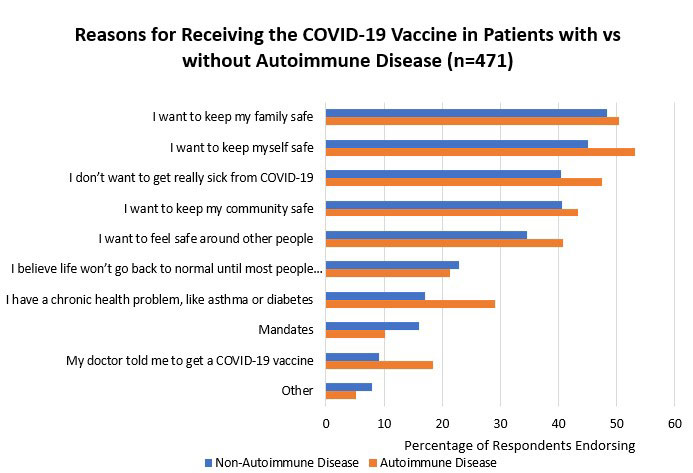
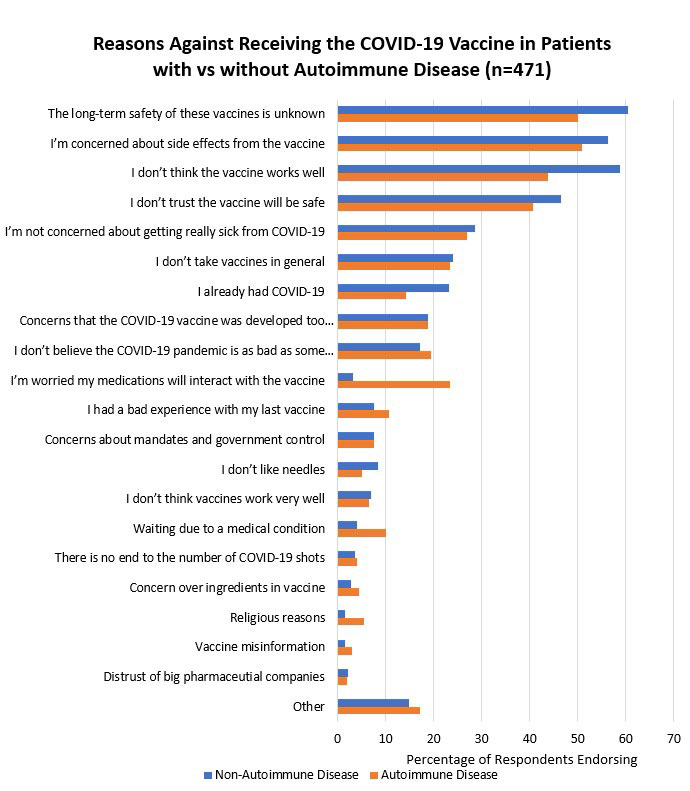
Results: The number of reasons for (β=-0.63, 95%CI[-0.43, -0.33]) and against the COVID-19 vaccine (β=0.28, 95%CI[0.10, 0.17]) was highly associated with decreased and increased vaccine hesitancy respectively. The factors most associated with decreased hesitancy were protecting family (β=-0.13, 95%CI[-0.90, -0.01]), personal safety (β=-0.27, 95%CI[-1.41, -0.45]), and preventing serious infection (β=-0.26, 95%CI[-1.31, -0.53]). Reasons associated with increased vaccine hesitancy were not being concerned about COVID-19 infection (β=0.14, 95%CI[0.25, 0.77]), concerns over vaccine safety (β=0.17, 95%CI[0.35, 0.87]), and believing the vaccine was made too quickly (β=0.07, 95%CI[0.04, 0.60]). While diagnosis of autoimmune disease was not associated with vaccination likelihood (β=-0.04, 95%CI[-0.34, 0.09]), autoimmune disease patients were more likely to cite having a chronic condition (29.1% vs 17.1%, p=0.003) and physician recommendations (18.4% vs 9.1%, p=0.005) as reasons to receive vaccination. Autoimmune disease patients were also more concerned about potential medication interaction with the vaccine (22.4% vs 3.3%, p< 0.001).
Conclusion: In our model, autoimmune disease did not directly change the COVID-19 vaccination likelihood. Instead, the number of benefits of vaccination identified by respondents strongly related to vaccination likelihood. The effect size of the benefits was more than double that of the cons of vaccine. For patients with autoimmune disease, provider recommendation to receive vaccine correlated with increased vaccination likelihood. Clinical conversations centered on the benefits of COVID-19 vaccination may help increase vaccine acceptance.
To cite this abstract in AMA style:
Gong J, Barnboym E, O'Mara m, Gurevich N, Mattar M, Anthony D, Perzynski A, Singer N. Key Self-reported Determinants of COVID-19 Vaccine Acceptance Among Persons with and Without Autoimmune Disease [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/key-self-reported-determinants-of-covid-19-vaccine-acceptance-among-persons-with-and-without-autoimmune-disease/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/key-self-reported-determinants-of-covid-19-vaccine-acceptance-among-persons-with-and-without-autoimmune-disease/