Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: SLE is an autoimmune rheumatic disease that contributes to increased morbidity and mortality due to multi-organ involvement, infections, and accelerated atherosclerosis leading to cardiovascular diseases. The Centers for Disease Control and Prevention (CDC) reported the worsening trends of SLE deaths from 1979-to 1998 along with gender, age, and race disparities followed by an improvement in mortality thereafter. The literacy level, differences in quality of care, and socioeconomic and environmental factors were proposed explanations for regional/racial mortality differences. The nationwide population-based studies for most recent mortality trends are lacking. We aimed to analyze the temporal trends of SLE-related mortality and review regional, gender, and racial variations across the different United States (US) census regions from 2001-to 2020.
Methods: The underlying cause of death data across the US was retrieved from the CDC’s Wide-Ranging Online Data for Epidemiologic Research (WONDER) database from 2001-to 2020. WONDER database reports the mortality data based on death certificates for US residents. The duration was stratified into five-year periods. The diagnosis of SLE using ICD-10 code M32 was queried among female and male gender without age restrictions. Age-adjusted mortality rate (AAMR) per 100,000 population was calculated for the four US census regions (CR1 Northeast, CR2 Midwest, CR3 South, and CR4 West), and different racial groups.
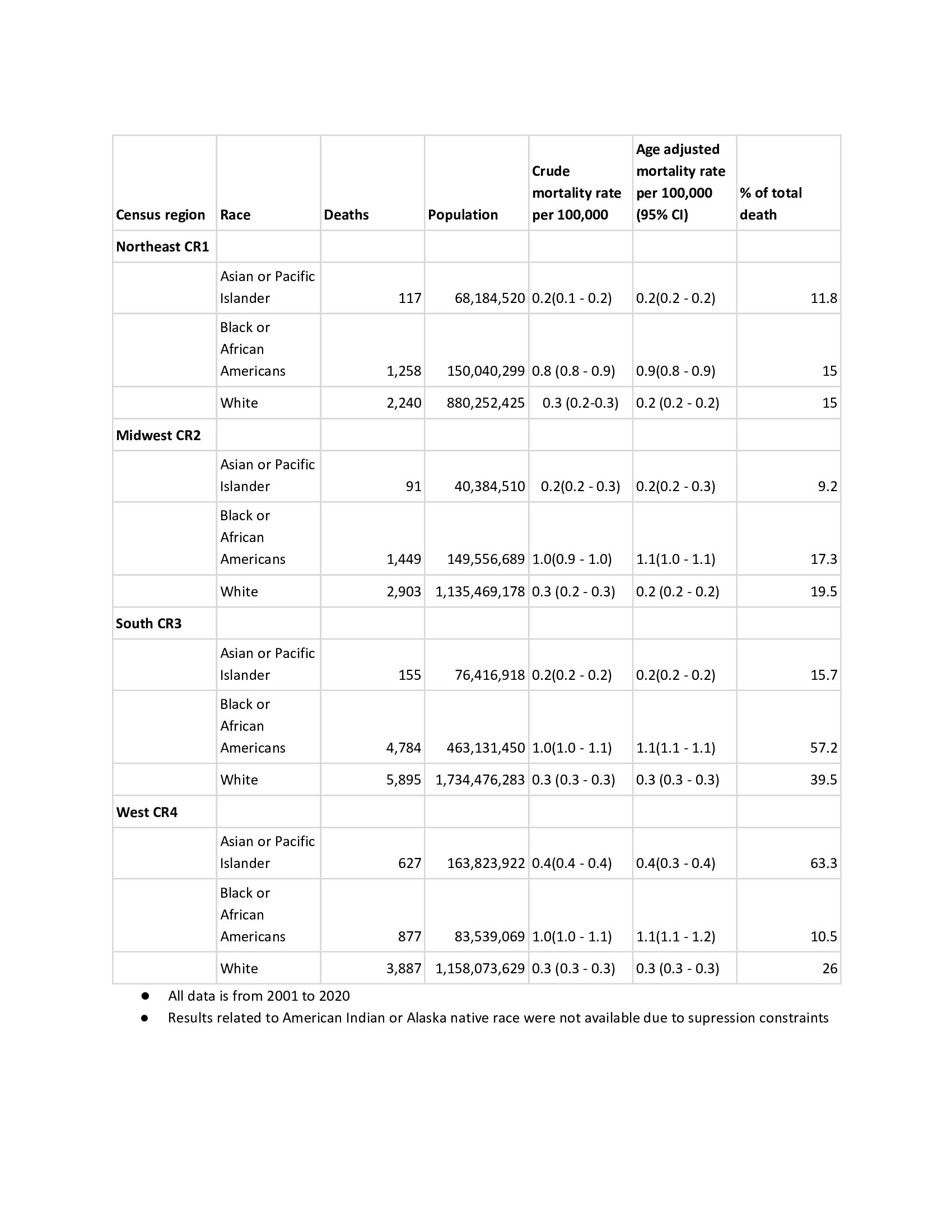
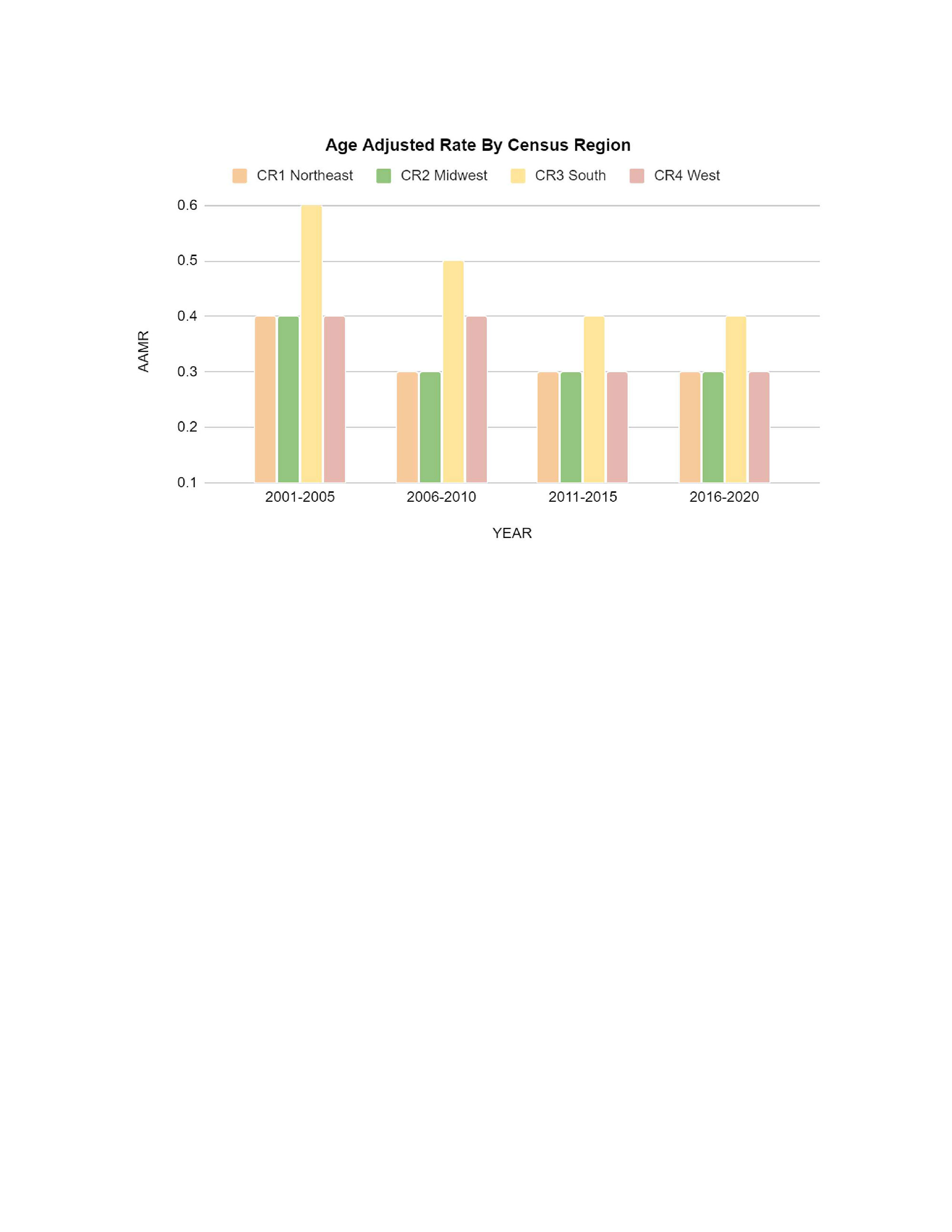
Results: From 2001-to 2020, a total of 24,552 deaths were attributed to SLE with a decline from 6670 (2001-2005) to 5958 (2016-2020). Overall, AAMR per 100,000 deaths declined by 40% during the study period. The regional AAMR declined by 25% each in the Northeast, Midwest, and West. The maximum decline was observed in the South by 33%. However, overall AAMR remained higher in the South compared to the other census regions (Figure 1). Women had higher Age-Adjusted mortality than men with a downward trajectory reported in all regions; a decline in 50%, 17%, 22%, and 29% in females AAMR in CR1, CR2, CR3, and CR4 respectively over the study duration (Table 1). African Americans had a higher AAMR during these two decades in all census regions than Whites and Asians (Table 2).
Conclusion: This analysis shows an overall and regional decline in deaths from SLE from 2001- to 2020. However, there has been no change in the AAMR in the Northeast and Midwest over the past 15 years, and over the past 10 years in the South and West despite the improvement in therapeutics; a possible explanation can be changing SLE incidence over time. The persistence of geographic, racial, and gender disparities among different census regions, and no decline in mortality in the last 10-15 years are concerning and warrant further investigation. The study limitations include death certificate errors leading to changes in mortality statistics and underreporting SLE as a cause of death.
To cite this abstract in AMA style:
Kaur I, Jagdey H, Mirza h, Mughal W, Bansal P. The Mortality Trends Related to SLE in the United States – A 20-year Analysis (2001-to 2020) from the WONDER Database [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/the-mortality-trends-related-to-sle-in-the-united-states-a-20-year-analysis-2001-to-2020-from-the-wonder-database/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-mortality-trends-related-to-sle-in-the-united-states-a-20-year-analysis-2001-to-2020-from-the-wonder-database/