Session Information
Date: Saturday, November 12, 2022
Title: Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster I
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Diagnostic delays are common with psoriatic arthritis (PsA), and screening surveys for identifying at-risk patients are infrequently used in busy clinical practices. We previously demonstrated that patients with psoriasis were more frequently evaluated by a rheumatologist if they screened positively on a home screening survey and then contacted study staff directly for a rheumatology appointment. This method bypassed an initial screening by their primary doctors. In this sub-analysis, we sought to characterize the patient findings during the initial rheumatologic evaluation. Our goal was to determine whether their referral to rheumatology was clinically appropriate.
Methods: Within the University of Utah and VA Medical Center healthcare systems in Salt Lake City, patients with an International Classification of Diseases (ICD) code for psoriasis but not PsA in the electronic health record (EHR) were identified. The Psoriasis Epidemiology Screening Tool Survey1 was disseminated electronically and via postal mail beginning 9/18/20 (index date). Patients that screened positively were instructed to contact study staff for a rheumatology appointment. Patient characteristics, clinical findings and diagnostic outcomes were extracted from the EHR beginning 2/2/22. A rheumatology referral was deemed appropriate if the patient had: (1) a history of confirmed or probable psoriasis; and (2) no previous encounters with a rheumatologist within the last 6 years. They also had to have: (3) a diagnosis of PsA; OR (4) symptoms, examination findings or test results that warranted an additional workup or a rheumatology follow-up.
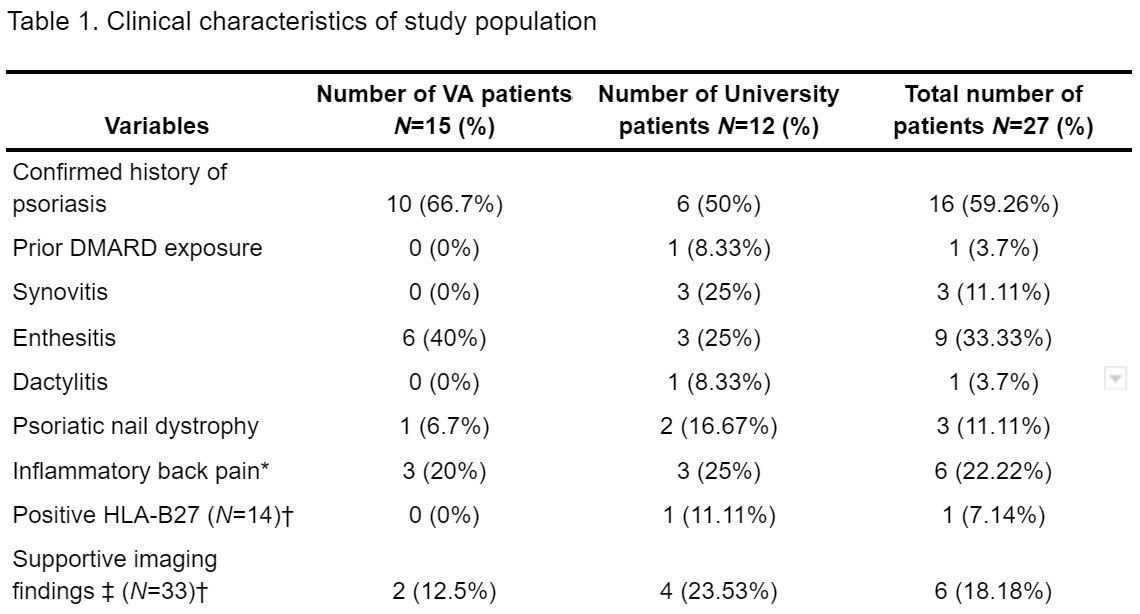
Results: The population included 1,413 patients, of whom 27 were seen by a rheumatologist. 66.6% were male with a mean age of 61.5. 14.8% had a previous encounter with a rheumatologist that was nondiagnostic for PsA. 59.2% had a verified history of psoriasis by a dermatologist or primary care provider. The most common clinical finding was enthesitis (33.3%) of the Achilles, plantar fascia insertions or epicondyles (Table 1). PsA diagnosis occurred in 4.7%. An additional 6.7% were diagnosed with possible PsA or another inflammatory joint disease (Figure 1). The rheumatology referral was deemed appropriate in 63%.
Conclusion: With patient-driven PsA screening and rheumatology referrals, over half of the referrals were deemed appropriate. The rate of misdiagnosed psoriasis was high due to inaccurate ICD code data. While the rate of PsA diagnosis was low, a dedicated evaluation by a rheumatologist in this at-risk population can provide reassurance and valuable patient education. There is also a highly beneficial impact for those who were diagnosed with PsA. Patient engagement may improve with future study cohorts (n≈24,000 patients), as the impacts of the COVID-19 pandemic decline and adjustments are made to engagement strategies.
1Ibrahim GH, et al. Clin Exp Rheumatol. 2009; 27:469-74.
To cite this abstract in AMA style:
Meier M, Walsh J. Direct to Patient Screening of Psoriatic Arthritis: Clinical Findings and Outcomes of Patient-Driven Rheumatology Referrals [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/direct-to-patient-screening-of-psoriatic-arthritis-clinical-findings-and-outcomes-of-patient-driven-rheumatology-referrals/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/direct-to-patient-screening-of-psoriatic-arthritis-clinical-findings-and-outcomes-of-patient-driven-rheumatology-referrals/