Session Information
Date: Tuesday, November 9, 2021
Title: Abstracts: Spondyloarthritis Including PsA – Diagnosis, Manifestations, & Outcomes II (1919–1922)
Session Type: Abstract Session
Session Time: 2:30PM-2:45PM
Background/Purpose: Psoriatic Arthritis (PsA) typically affects peripheral joints, but in some patients the disease can involve the spine. While magnetic resonance imaging (MRI) is an important diagnostic tool for spondyloarthritis, especially in early phases, there is minimal information about MRI features of axial PsA.
The purpose of the study was to describe the prevalence of inflammatory and structural lesions by whole-spine MRI in patients with psoriatic disease, and assess the correlation of MRI-defined spondyloarthritis (MRI-SpA) with clinical and laboratory features and with classification criteria for axial spondyloarthritis (axSpA).
Methods: In this retrospective analysis we included 93 patients selected from 2 populations: 1) 41 patients with active PsA, who were referred for a whole-spine MRI irrespective of whether they had axial symptoms, and 2) 52 patients with psoriasis and suspected or confirmed PsA who were referred to a whole-spine MRI for suspected axPsA. Patients on biologic advanced therapies were excluded.
Clinical, radiographic and laboratory data were analyzed. Inflammatory back pain (IBP) was defined according to 3 criteria: Berlin, Assessment of Spondyloarthritis International Society (ASAS) and rheumatologist impression.
MRI scans of the sacroiliac joints and whole-spine (T1W and STIR) were assessed by a musculoskeletal radiologist blinded to the clinical and radiographic data. MRI-SpA was defined as: 1) ASAS consensus for active spondylitis/sacroiliitis, and 2) the radiologist impression (considering inflammatory and structural lesions).
The agreement between MRI-SpA as a gold standard, and the ASAS classification criteria for axSpA and different definitions of IBP was assessed. Logistic regression evaluated the association between MRI-SpA and clinical, demographic and laboratory factors.
Results: 93 patients were analyzed (mean age 43.3 ±13, 52.7% women, Table 1). The prevalence of HLA-B*27 was 10.9%. Axial symptoms were present in 81.7%, being defined as IBP in 36.6%/36.6%/57% according to Berlin, ASAS and rheumatologist criteria, respectively. MRI-SpA was found in only 9 (9.7%) patients by ASAS definition and 12 (12.9%) by radiologist impression.
Overall, low agreement was found between the three IBP definitions and MRI-SpA (Table 2). IBP by rheumatologist impression was the most sensitive (50-56%) and ASAS and Berlin criteria for IBP were most specific (62-63%). Poor sensitivity was found for the ASAS criteria for axSpA and MRI-Spondylitis (ASAS definition 22.2%; radiologist impression 25%, Fig. 1). Onset of axial pain after the age of 40 and absence of axial pain accounted for most patients with MRI-SpA not meeting the ASAS axSpA criteria or IBP criteria. Male sex was associated with MRI-Spondylitis (OR 6.9; 95% CI 1.4, 33.6) in multivariable regression analysis.
Conclusion: The overall prevalence of axial inflammatory and structural spondylitis by whole-spine MRI was low despite the high prevalence of axial symptoms. Poor correlation was found between imaging and clinical findings highlighting the need for further research of the underlying mechanisms of axial involvement in PsA.
 * Patients with active PsA who were referred for a whole-spine MRI regardless of axial symptoms. † Patients with psoriasis and confirmed or suspected PsA, referred for a whole-spine MRI due to suspected axial PsA. ‡ At least 1 syndesmophyte. § Spondylitis and/or sacroiliitis according to ASAS. (Spondylitis: anterior/posterior BME in ≥3 sites / fatty lesions at several sites. Active sacroiliitis: ≥2 BME lesions on a single SIJ slice and/or ≥ 1 BME lesion on 2 consecutive slices.) ¶ Spondylitis and/or sacroiliitis according to radiologist impression (considering inflammatory and structural lesions).
* Patients with active PsA who were referred for a whole-spine MRI regardless of axial symptoms. † Patients with psoriasis and confirmed or suspected PsA, referred for a whole-spine MRI due to suspected axial PsA. ‡ At least 1 syndesmophyte. § Spondylitis and/or sacroiliitis according to ASAS. (Spondylitis: anterior/posterior BME in ≥3 sites / fatty lesions at several sites. Active sacroiliitis: ≥2 BME lesions on a single SIJ slice and/or ≥ 1 BME lesion on 2 consecutive slices.) ¶ Spondylitis and/or sacroiliitis according to radiologist impression (considering inflammatory and structural lesions).
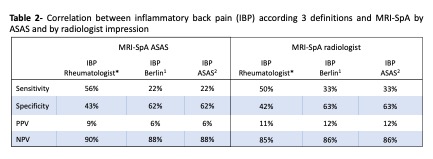 * Inflammatory back pain according to rheumatologist impression at the clinical visit (considering symptoms but no images) 1. Rudwaleit M, et al. Arthritis Rheum. 2006;54(2):569-78. 2. Sieper J, et al. Ann Rheum Dis. 2009;68(6):784-8.
* Inflammatory back pain according to rheumatologist impression at the clinical visit (considering symptoms but no images) 1. Rudwaleit M, et al. Arthritis Rheum. 2006;54(2):569-78. 2. Sieper J, et al. Ann Rheum Dis. 2009;68(6):784-8.
 *Spondylitis and/or sacroiliitis according to ASAS/OMERACT definitions (Spondylitis: anterior/posterior BME in ≥ 3 sites / fatty lesions at several sites. Sacroiliitis: ≥ 2 BME lesions on a single SIJ slice and/or ≥ 1 BME lesion on 2 consecutive slice). † Spondylitis and/or sacroiliitis according to radiologist impression (considering inflammatory and structural lesions)
*Spondylitis and/or sacroiliitis according to ASAS/OMERACT definitions (Spondylitis: anterior/posterior BME in ≥ 3 sites / fatty lesions at several sites. Sacroiliitis: ≥ 2 BME lesions on a single SIJ slice and/or ≥ 1 BME lesion on 2 consecutive slice). † Spondylitis and/or sacroiliitis according to radiologist impression (considering inflammatory and structural lesions)
To cite this abstract in AMA style:
Diaz P, Eshed I, Feld J, Eder L. Axial Psoriatic Arthritis: Correlation Between Whole Spine MRI Abnormalities and Clinical Findings [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/axial-psoriatic-arthritis-correlation-between-whole-spine-mri-abnormalities-and-clinical-findings/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/axial-psoriatic-arthritis-correlation-between-whole-spine-mri-abnormalities-and-clinical-findings/
