Session Information
Date: Monday, November 8, 2021
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Uveitis is the most frequent extra-musculoskeletal manifestation in Spondyloarhtritis (SpA). Moreover, up to 50% of patients with an acute episode of uveitis develop recurrent anterior uveitis. Recently, the prevalence of history of uveitis reported in ASAS perSPA study (PERipheral involvement in SpondyloArthritis) was similar in axial and peripheral SpA (21.6% and 17.3%, respectively). However, it is not well known whether the clinical characteristics of patients with uveitis and recurrent uveitis differ between patients with axial and peripheral SpA. The primary objective was to compare the clinical characteristics of axial and peripheral SpA patients who have ever suffered from uveitis. Secondary objective was to compare the clinical characteristics of axial and peripheral SpA patients with a single episode of uveitis versus SpA patients with recurrent uveitis.
Methods: This is a post-hoc analysis of the ASAS-PerSpA study which included 3465 patients with SpA, 2910 patients fulfilling ASAS axSpA criteria and 555 patients fulfilling peripheral ASAS criteria. Recurrent uveitis was defined as the presence of 2 or more episodes of uveitis ever. Univariable and multivariable binary logistic regression analyses were conducted to identify factors associated with the presence of uveitis ever and the presence of recurrent uveitis.
Results: In the multivariable analysis, the presence of uveitis was significantly associated with the presence of HLA-B27 and disease duration, OR 2.88 (CI95% 2.15 – 3.91) and OR 1.05 (CI95% 1.04 – 1.06) respectively. Furthermore, the presence of inflammatory bowel disease ever is increased in patients with uveitis, OR 1.60 (CI95% 1.04 – 2.44). Nevertheless, the presence of psoriasis is decreased in patients with uveitis, OR 0.43 (CI95% 0.31 – 0.59). Patients from Latin America region were more likely to present uveitis in comparison with European patients, OR 1.42 (CI95% 1.02 – 1.94). Importantly, the presence of uveitis was not significantly different in patients with axSpA as compared to patients with pSpA (Figure 1). One the other hand, only disease duration and body mass index (BMI) was significantly associated with the presence of recurrent uveitis, OR 1.04 (CI95% 1.01-1.08) and OR 1.02 (CI95% 1.01-1.04) (Figure 2).
Conclusion: The prevalence of uveitis was not significantly higher in patients with axSpA as compared to patients with pSpA. HLA-B27 positivity is associated with the presence of uveitis, but not with recurrent uveitis in SpA patients. Hence, further biomarkers are needed to identify patients at risk of recurrent uveitis
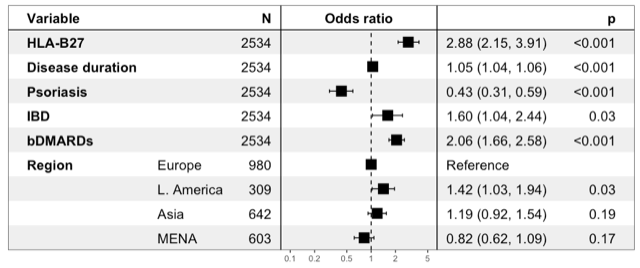 Figure 1. Multivariable analysis of 2534 patients with Spondyloarthritis to identify factors associated with the presence of uveitis ever. IBD, inflammatory bowel disease; HLA-B27, human leucocyte antigen B27; bDMARDs, biological disease-modifying antirheumatic drugs.
Figure 1. Multivariable analysis of 2534 patients with Spondyloarthritis to identify factors associated with the presence of uveitis ever. IBD, inflammatory bowel disease; HLA-B27, human leucocyte antigen B27; bDMARDs, biological disease-modifying antirheumatic drugs.
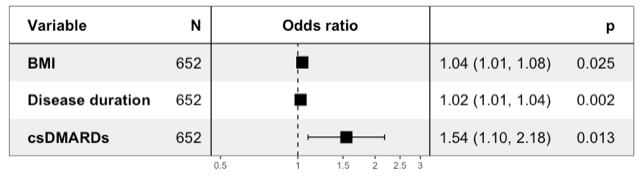 Figure 2. Multivariable analysis of 2534 patients with Spondyloarthritis to identify factors associated with the presence of recurrent uveitis. BMI, body mass index; csDMARDs, conventional synthetic disease-modifying antirheumatic drugs.
Figure 2. Multivariable analysis of 2534 patients with Spondyloarthritis to identify factors associated with the presence of recurrent uveitis. BMI, body mass index; csDMARDs, conventional synthetic disease-modifying antirheumatic drugs.
To cite this abstract in AMA style:
LLOP VILALTELLA M, moreno M, Arévalo M, Gratacós J, Dougados M, López Medina C. Uveitis in Spondyloarthritis Patients. Is There Any Specific Clinical Picture? [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/uveitis-in-spondyloarthritis-patients-is-there-any-specific-clinical-picture/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/uveitis-in-spondyloarthritis-patients-is-there-any-specific-clinical-picture/
