Session Information
Date: Saturday, November 6, 2021
Title: Miscellaneous Rheumatic & Inflammatory Diseases Poster I (0183–0209)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Cystoid Macular Edema (CME) is the most important cause of blindness in non-infectious uveitis (NIU) (1). Corticosteroids and conventional and/or biological immunosuppressant may be required (1-6). High-dose intravenous methylprednisolone (IVMP) pulse therapy may induce a rapid improvement.
The objective is to evaluate the efficacy and safety of IVMP pulse therapy in CME of different immune mediated inflammatory diseases (IMID).
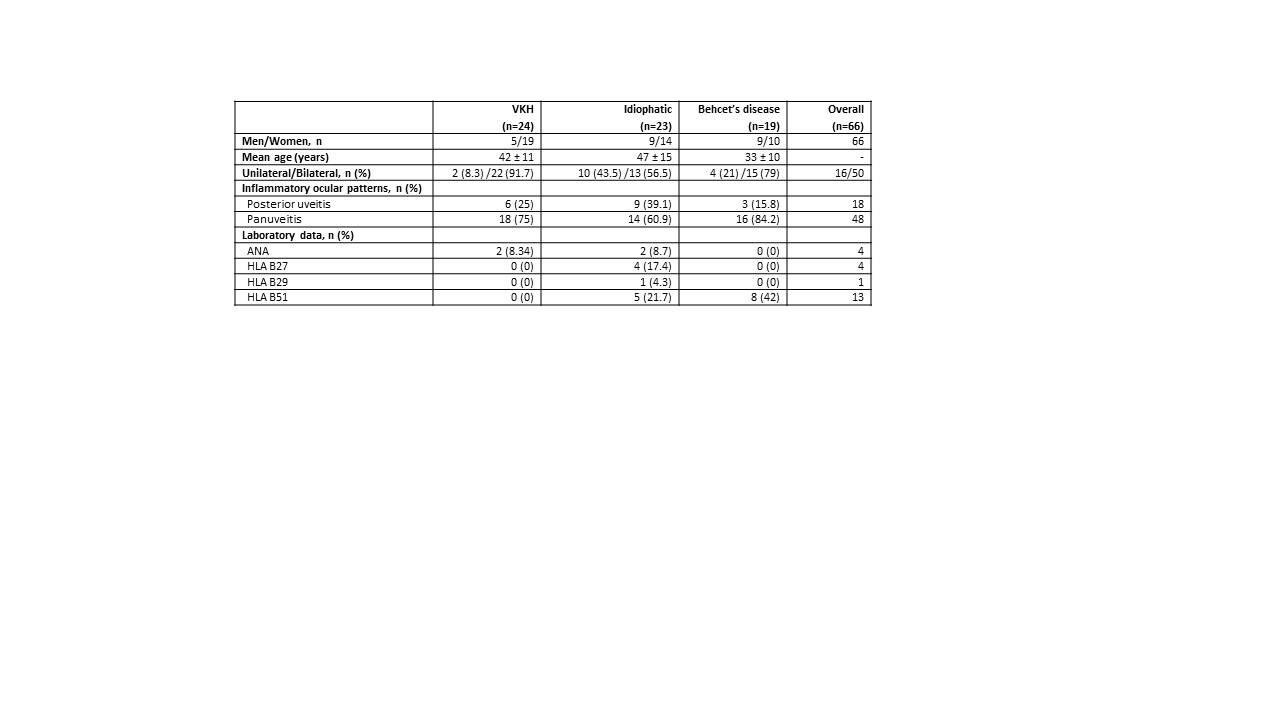
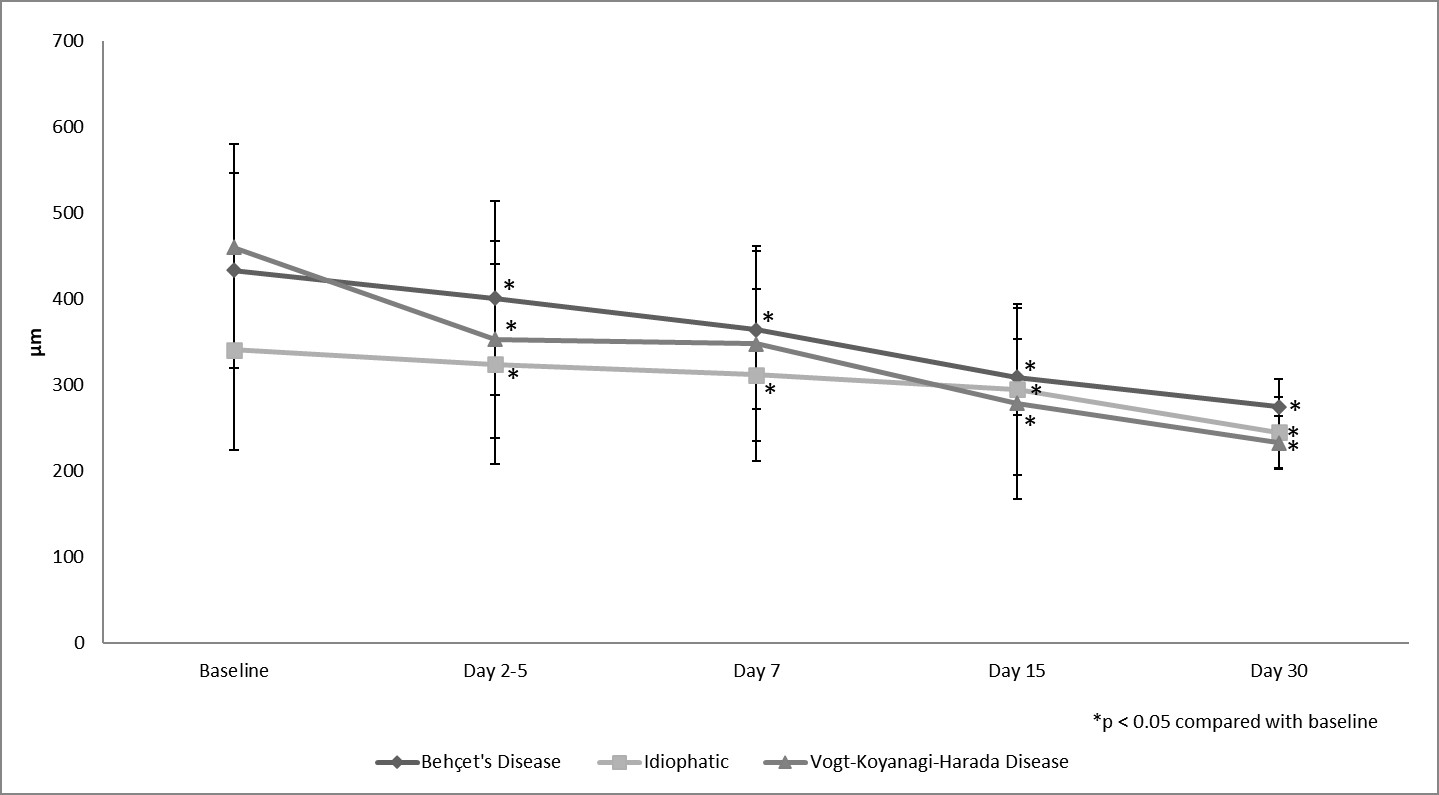
Methods: Multicentre study of 66 patients with severe ocular inflammation who received IVMP. The underlying diseases were: Vogt-Koyanagi-Harada disease (VKHD)(n=24), Behçet’s disease (BD) (19) and idiopathic NIU (23). The main outcome variable was macular thickness and macular edema (Optical coherence tomography [OCT] >300 μm); that was assessed at 0 (basal), 2-5, 7, 15 and 30 days after IVMP. The results are expressed as mean ±SD for normally distributed variables, or as median [IQR] when are not. Comparison of continuous variables was performed using the Wilcoxon test.
Results: We studied 43♀/ 23♂ patients. The main features are shown in TABLE. IVMP dose ranged from 250 to 1000 mg/day administered for 3-5 consecutive days, the dose was established according to the presence or not of other systemic manifestations apart from uveitis. All of them had active intraocular inflammation at the moment of the study. A rapid and maintained statistically improvement was observed in OCT values in all underlying diseases (FIGURE). No major side effects were observed.
Conclusion: High-dose IVMP pulse therapy is useful and safe in the prompt control of CME, regardless of the underlying IMID.
REFERENCES
1. Vegas-Revenga N, et al. Am J Ophthalmol. 2019; 200:85-94. doi: 10.1016/j.ajo.2018.12.019
2. Calvo-Río V, et al. Clin Exp Rheumatol. 2014;32(4 Suppl 84): S54-7. PMID: 25005576
3. Santos-Gómez M, et al. Clin Exp Rheumatol. 2016;34(6 Suppl 102): S34-S40. PMID:27054359
4. Atienza-Mateo B, et al. Rheumatology (Oxford) 2018;57(5):856-864. doi: 10.1093/rheumatology/kex480.
5. Atienza-Mateo B, et al. Arthritis Rheumatol. 2019; 71(12):2081-2089. doi: 10.1002/art.41026.
6. Martín-Varillas JL, et al. Ophthalmology. 2018;125(9):1444-1451. doi: 10.1016/j.ophtha.2018.02.020
To cite this abstract in AMA style:
Vegas-Revenga N, Martin-Varillas J, Calvo-Río V, Gonzalez-Mazon I, Sánchez-Bilbao L, Beltrán Catalán E, Fonollosa A, Blanco A, Blanco A, Cordero Coma M, Ortego N, Torre I, Hernandez F, Muñóz-Fernández S, Esteban-Ortega M, Diaz-Llopis M, Cañal J, Ventosa J, Demetrio-Pablo R, Dominguez Casas L, Castañeda S, Ferraz-Amaro I, gonzalez-Gay M, Blanco R. Rapid Improvement in Cystoid Macular Edema with High Dose Intravenous Methylprednisolone in Non-Infectious Uveitis of Different Immune Mediated Inflammatory Diseases [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/rapid-improvement-in-cystoid-macular-edema-with-high-dose-intravenous-methylprednisolone-in-non-infectious-uveitis-of-different-immune-mediated-inflammatory-diseases/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rapid-improvement-in-cystoid-macular-edema-with-high-dose-intravenous-methylprednisolone-in-non-infectious-uveitis-of-different-immune-mediated-inflammatory-diseases/