Session Information
Date: Monday, November 9, 2020
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: The diagnosis of axial spondyloarthritis (axSpA) is often delayed by several years and reducing that gap between symptom onset and diagnosis poses a major challenge in rheumatology. The objective of this study was to evaluate the diagnostic value of SpA parameters and their combination for the diagnosis of axSpA in patient populations with different a priori probabilities of this disease.
Methods: For the aim of the present analysis we used data from the Optimal Referral Strategy for Early Diagnosis of Axial Spondyloarthritis (OptiRef) study comprising a total of 361 patients who presented to a rheumatologist because of chronic back pain and suspicion of axSpA. Of those, 181 were referred by primary care physicians or orthopaedists and 180 patients were recruited via an online screening tool. All patients received a structured rheumatologic examination which included the evaluation of SpA features and resulted into a diagnosis of axSpA/no axSpA. Sensitivities, specificities, and likelihood ratios (LRs) for SpA features were determined in the entire group and in both subgroups with different referral pathways. The respective post-test probabilities of axSpA were calculated.
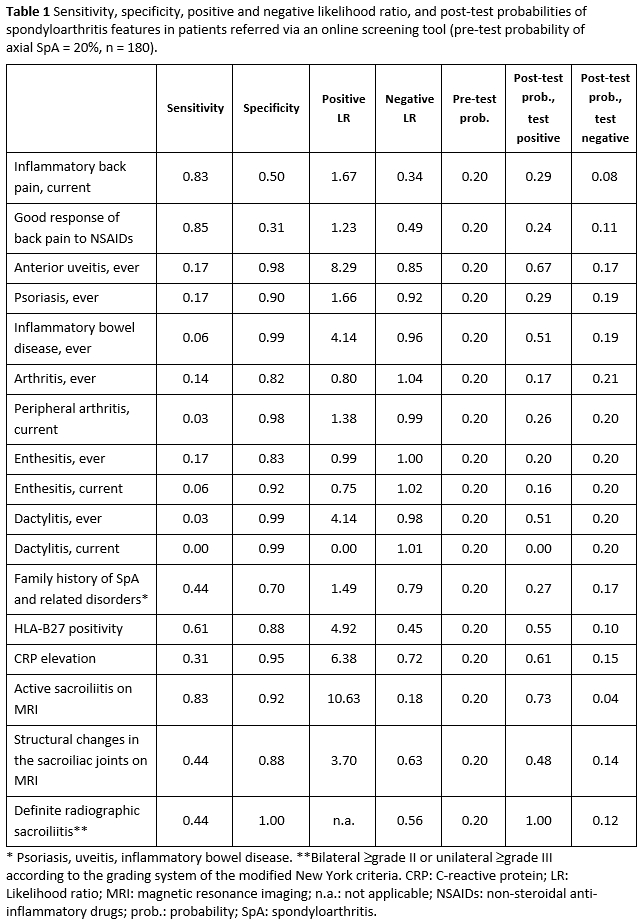
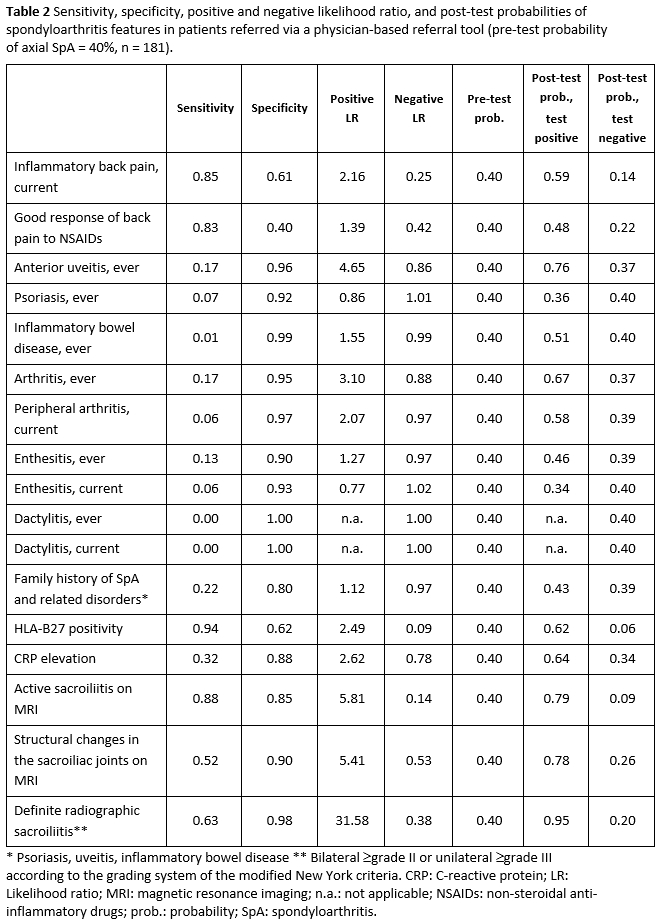
Results: The prevalence of axSpA was 30% in the entire group, 20% in the online screening subgroup and 40% in the physician-referred subgroup. These frequencies were used as pre-test probabilities in the calculation of the post-test probabilities among the respective groups. It could be shown that differences in the pre-test probability affect not only the post-test probability of the disease, but also the relative diagnostic value of single SpA features. For instance, the presence of inflammatory back pain increased the probability of the presence of axSpA from the background 20% to 29% in the online screening group (positive LR of 1.67) (Table 1) and from the background 40% to 59% in the physician-referred group (positive LR of 2.16) (Table 2), whereas its absence decreased the respective probabilities to 8% and 14%, respectively.
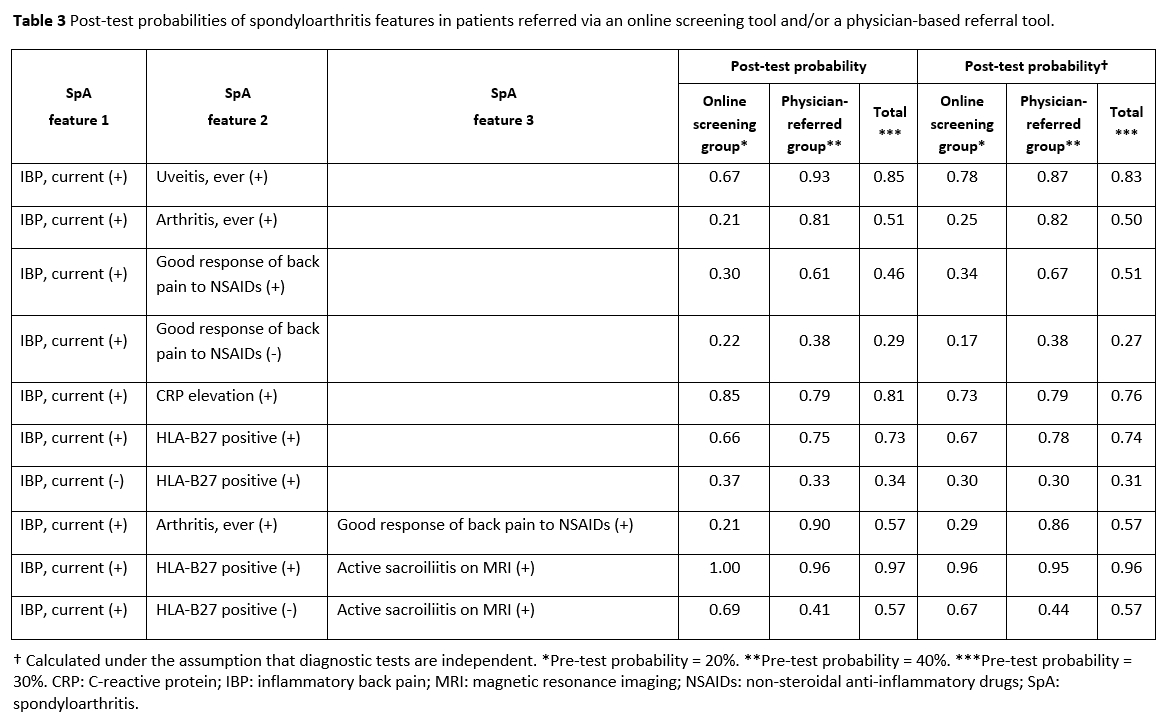
Furthermore, combinations of parameters performed differently in the studied groups. For instance, combining IBP with anterior uveitis did not increase the post-test probability for axSpA in the online screening group (it remained 67%), but in the physician-referred group (from 76% to 93%). Using HLA-B27 positivity and active sacroiliitis on MRI in combination with IBP resulted in a surge in the post-test probability of the presence of axSpA to over 95% in all groups (Table 3). Using a simplified formula to calculate the post-test probabilities for axSpA for combinations of parameters, which is based on the product of the respective LRs and holds if the diagnostic tests are independent, could lead to differences of more than 10% (Table 3).
Conclusion: The diagnostic value of SpA features is not fixed and may vary substantially depending on the characteristics of the patient group including their referral pathway and their pre-test probability of axSpA. This should be taken into account in the diagnostic approach of axSpA.
To cite this abstract in AMA style:
Poddubnyy D, Proft F, Sieper J, Redeker I. How to Diagnose Axial Spondyloarthritis in 2020? A Data-Driven Estimation of the Disease Probability in Patients with a priori Different Likelihoods of the Diagnosis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/how-to-diagnose-axial-spondyloarthritis-in-2020-a-data-driven-estimation-of-the-disease-probability-in-patients-with-a-priori-different-likelihoods-of-the-diagnosis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/how-to-diagnose-axial-spondyloarthritis-in-2020-a-data-driven-estimation-of-the-disease-probability-in-patients-with-a-priori-different-likelihoods-of-the-diagnosis/