Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The mainstay of treatment for vasculitis has been corticosteroids and other cytotoxic and immunosuppressive medications (e.g., cyclophosphamide, methotrexate) to promptly achieve and maintain remission. Novel treatment options for giant cell arteritis and some forms of polyangiitis have recently become available, however unmet need remains. The purpose of this study is to explore the real world use of biologic agents with different mechanisms of action in patients with Behçet’s disease and other rare systemic vasculitides, despite a paucity of regulatory-approved options.
Methods: The OM1 Real World Data Cloud (OM1, Boston, MA), which collects, links and leverages structured and unstructured data from electronic medical records (EMR), claims and other sources in an ongoing and continuously updating manner in the US, was used for the analysis. Use of anti-TNFs, anti-IL-6 agents and other select biologic disease-modifying anti-rheumatic drugs (DMARDs) and monoclonal antibodies between January 2013 and April 2020 were evaluated in patients diagnosed with Behcet’s disease (BD), Takayasu’s arteritis (TA), polyarteritis nodosa (PAN), mixed cryoglobulinemia (MC), granulomatosis with polyangiitis (GPA), eosinophilic granulomatosis with polyangiitis (EGPA) and microscopic polyangiitis (MPA). For the DMARDs, patients with a documented diagnosis of one or more FDA-approved indications for each DMARD were excluded. By excluding patients with comorbidities (e.g., rheumatoid arthritis) included in the marketed indications for each agent, some patients for whom the agent was specifically used for vasculitis may have been omitted. Patients may have been treated with more than one biologic of interest.
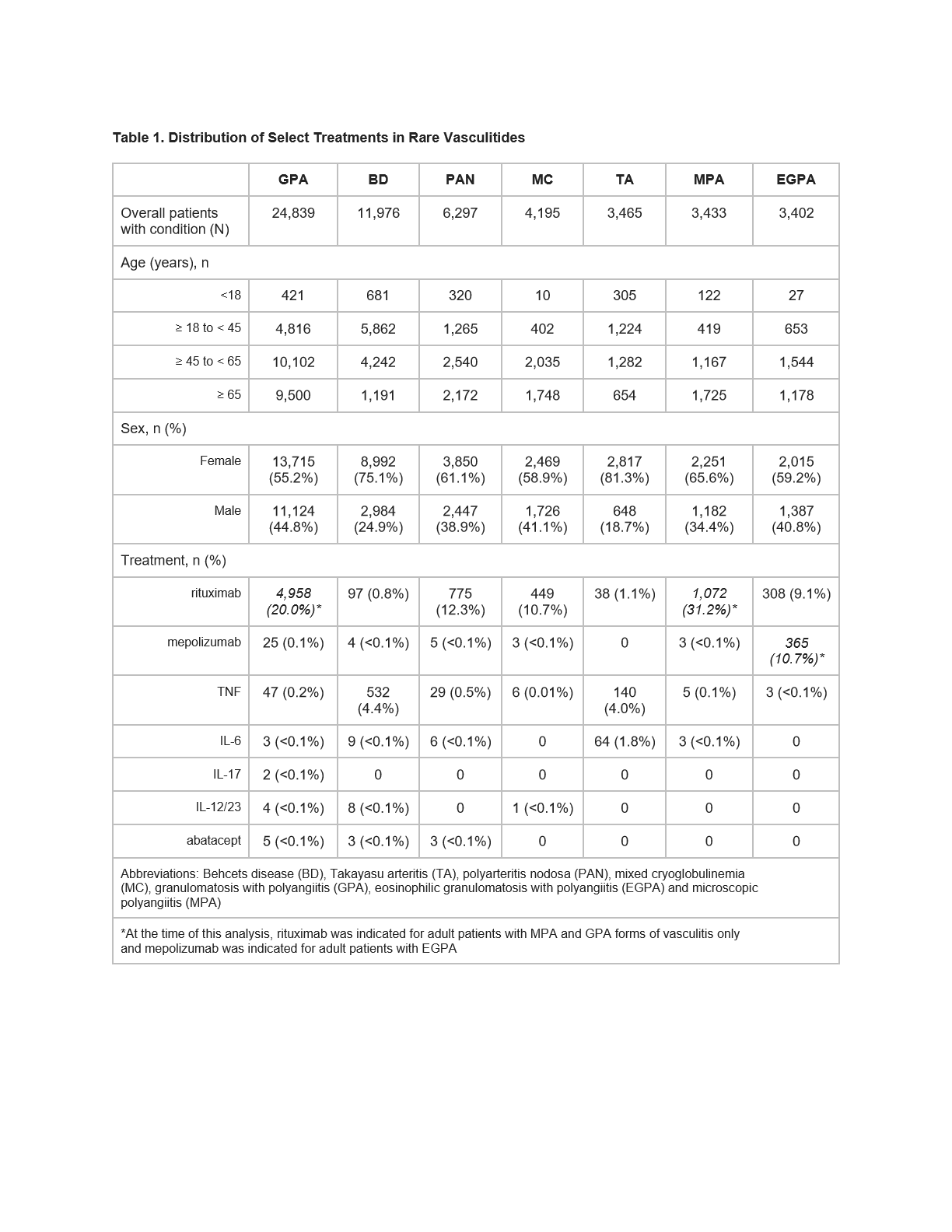
Results: Overall, > 50,000 patients diagnosed with the vasculitides of interest were identified, with GPA and BD the most common (Table 1). Across the conditions of interest, the majority were female (62.7%). A small proportion of pediatric patients were identified. Amongst patients with BD, anti-TNFs were the most commonly used biologic (n=532, 4.4% of BD patients) followed by rituximab. While rituximab was frequently used in its indicated forms (GPA and MPA), it was also used across the other forms of vasculitis. Anti-TNF and anti-IL-6 use was noted in 140 (4.0%) and 64 (1.8%) of TA patients, respectively; rituximab was less commonly used. The other DMARDs evaluated were rarely observed.
Conclusion: If left untreated (or under-treated), systemic vasculitides can result in substantial multisystem morbidity. As the proinflammatory activity in the vasculitides involves many aspects of the immune system, it remains unclear which mechanism of action is best suited in an individualized treatment setting. Harnessing real world experience may help inform clinical practice, including decisions to switch therapies, and clinical trial design.
To cite this abstract in AMA style:
Starzyk K, Milberg K, Deshpande A, Curhan G. An Evaluation of Real World Use of Biologics in Rare Systemic Vasculitides During Routine Clinical Care in the US [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/an-evaluation-of-real-world-use-of-biologics-in-rare-systemic-vasculitides-during-routine-clinical-care-in-the-us/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/an-evaluation-of-real-world-use-of-biologics-in-rare-systemic-vasculitides-during-routine-clinical-care-in-the-us/