Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Comorbidities
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Post-traumatic stress disorder (PTSD), the sentinel stress-related mental disorder, may be associated with increased risk of developing autoimmune disease, including systemic lupus erythematosus (SLE). This study aimed to study the relationship between PTSD and risk of SLE in a large, diverse population of Medicaid enrollees. We hypothesized patients with incident SLE would be more likely to have a prior diagnosis of PTSD than those without SLE.
Methods: We performed a case-control study using patients ages 18 to 65 years old in the Medicaid Analytic eXtract (MAX) database between January 1, 2007 and December 31, 2010. Cases of SLE were defined as having >3 ICD-9 codes for SLE from hospital discharge diagnoses or physician visit claims, occurring at least 30 days apart. Index date was defined as the date of the first code for SLE. Controls were matched to SLE cases for age, sex and race using a 1:10 ratio. Controls were patients without any claims for SLE, but who had another inpatient or outpatient claim in Medicaid on the SLE index date of the matched case. Exclusion criteria included having less than 12 months of continuous Medicaid enrollment prior to the index or matched control date. The exposure was PTSD, defined as having >2 ICD-9 codes for PTSD on different dates within 4 months of each other, occurring prior to the index date for SLE (Gravely, 2011; PPV 82%). We used conditional logistic regression to calculate the odds ratio (OR) and 95% confidence interval (CI) for history of PTSD prior to index date in cases vs. controls. Finally, we used multivariable analysis to adjust for variables collected prior to the index date, including area-level socioeconomic status (SES), smoking, obesity, oral contraception use, and time enrolled in Medicaid.
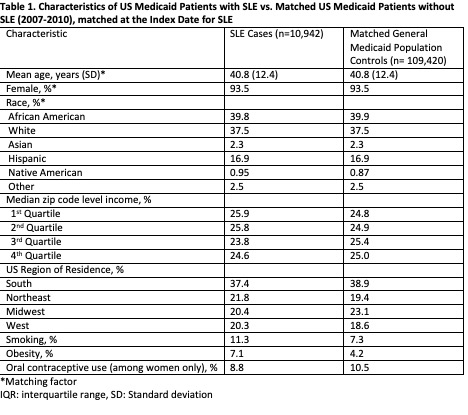
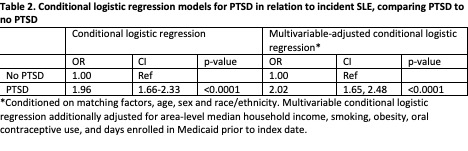
Results: We identified 10,942 cases of incident SLE, who were matched to 109,420 controls. There were significant differences at the index date in several characteristics, including zip code level income as a measure of socioeconomic status (SES), US region of residence, smoking, obesity, and oral contraceptive use (Table 1). 1.46% of Medicaid enrollees with SLE met the definition of PTSD prior to the index date, compared to 0.75% of controls (p< 0.001). The OR for PTSD and risk of incident SLE was 1.96 (95% CI 1.66-2.33, p< 0.001) in conditional logistic regression, and 2.02 (95% CI 1.65-2.48, p< 0.001) after multivariable adjustment (Table 2). Further adjustment for the matching factors did not alter risk estimates.
Conclusion: In this large, racially and sociodemographic diverse US patient population, we found a near doubling of odds of SLE associated with prior PTSD diagnosis. Chronic stress leading to hypothalamic-pituitary axis dysregulation and inflammatory cytokine upregulation are postulated mechanisms. Future studies are needed with longer follow-up time to clarify the underlying pathophysiology and characterize modifying influences in the relationship between PTSD and SLE.
To cite this abstract in AMA style:
Case S, Feldman C, Guan H, Kubzansky L, Koenan K, Costenbader K. Post-Traumatic Stress Disorder (PTSD) and Risk of Systemic Lupus Erythematosus (SLE) Among Medicaid Recipients [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/post-traumatic-stress-disorder-ptsd-and-risk-of-systemic-lupus-erythematosus-sle-among-medicaid-recipients/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/post-traumatic-stress-disorder-ptsd-and-risk-of-systemic-lupus-erythematosus-sle-among-medicaid-recipients/