Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Comorbidities
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The latest 2019 Lupus Classification criteria score (CCS) is based on weighted criteria and has been shown to predict 10-year mortality1. Our previous study also suggests that lupus score greater than 19 increases the risk of future hospitalizations2. We attempt to test the hypothesis that 2019 lupus classification criteria score can predict the cost of future hospitalizations.
Methods: Retrospective chart review was done at University of Kentucky (UK) between 2013 – 2019 to ascertain risk factors for hospitalization of lupus patients2. Post hoc analysis was applied to calculate cost of care.
Inclusion criteria: At least 3 outpatient rheumatology visits at UK with an ICD 9/10 diagnosis code for Lupus. Total of 217 patients met the inclusion criteria and 42 patients were hospitalized. 2019 Lupus classification score was calculated from first outpatient rheumatology visit. Total hospitalization cost was calculated by using hospital expense data3. Hospital expense data avoided variability of charges and reimbursement based on the type of insurance.
Results: Among 42 patients hospitalized, 26 (62%) were hospitalized within 2 years of their index rheumatology visit (Figure 1). Of 26, 15 were hospitalized due to lupus related causes with total mean hospital cost of 20426 usd. 11 patients were hospitalized unrelated to lupus with total mean cost of 17060 usd.
Patients whose 1st hospitalization was after 2 years of their index visit showed a trend toward overall lower mean hospitalization cost: 11370 usd as compared to patients hospitalized earlier than 2 years: 21065 usd (p value: 0.05). In addition, later hospitalization cost showed strong linear correlation with lupus score (r: 0.68, p value: 0.003) (Figure 2).
Patients who scored > 19 on the lupus CCS had almost twice the cost (28725 usd) due to inpatient hospitalization as compared to patients with CCS 19 or less in the subsequent two years of their index visit. In analysis of hospitalization any time after their index visit rather than the initial 2 years, patients with higher lupus score ( >19) still incurred higher cost compared to those with a lower CCS score (23841 usd vs 11490 usd, p < 0.07) (Table 1).
Conclusion: Our study found that late first hospitalization expense (1st hospitalization after 2 years of index visit) correlate well with the lupus score (p value: 0.05). In addition, higher lupus score ( > 19) increased hospitalization cost almost twofold as compared to lupus score 19 or less. These data could help to create models using 2019 Lupus classification criteria scores as a surrogate to predict future lupus hospitalization and cost of care, supporting Interventions designed to bring the cost down.
References:-
- Carneiro et.al; A comparison of three classification criteria sets for Systemic Lupus Erythematosus – a study looking at links to outcome and mortality; Arthritis Care Res (Hoboken)2019 Sep 10. doi: 10.1002/acr.24061
- Suman et.al; 2019 Lupus Classification Criteria Score Predicts Future Lupus Hospital Admission, Accepted abstract, EULAR 2020
- Trendwatch Chartbook 2018, American Hospital Association
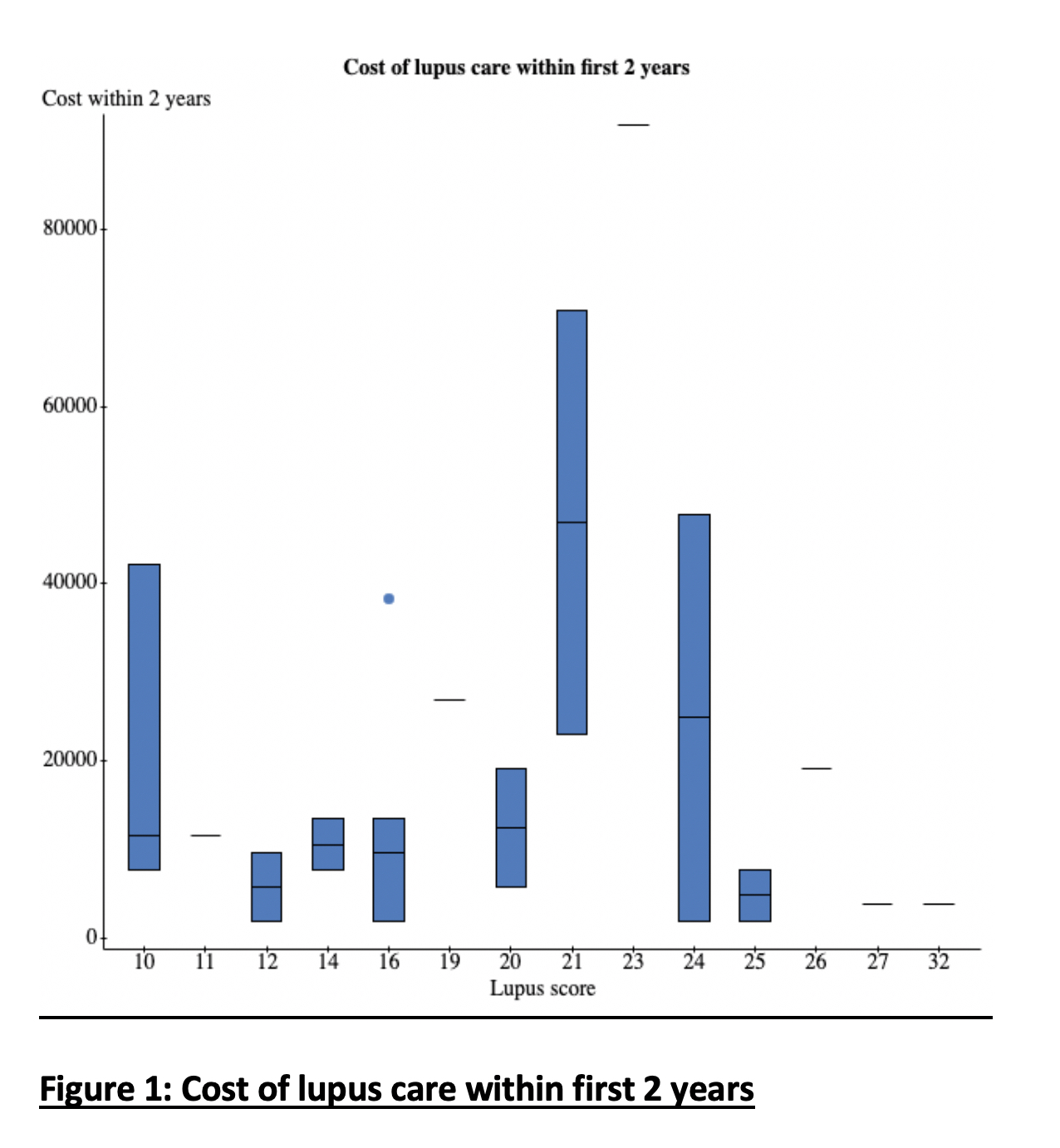 Figure 1: Cost of Lupus Care within first 2 years
Figure 1: Cost of Lupus Care within first 2 years
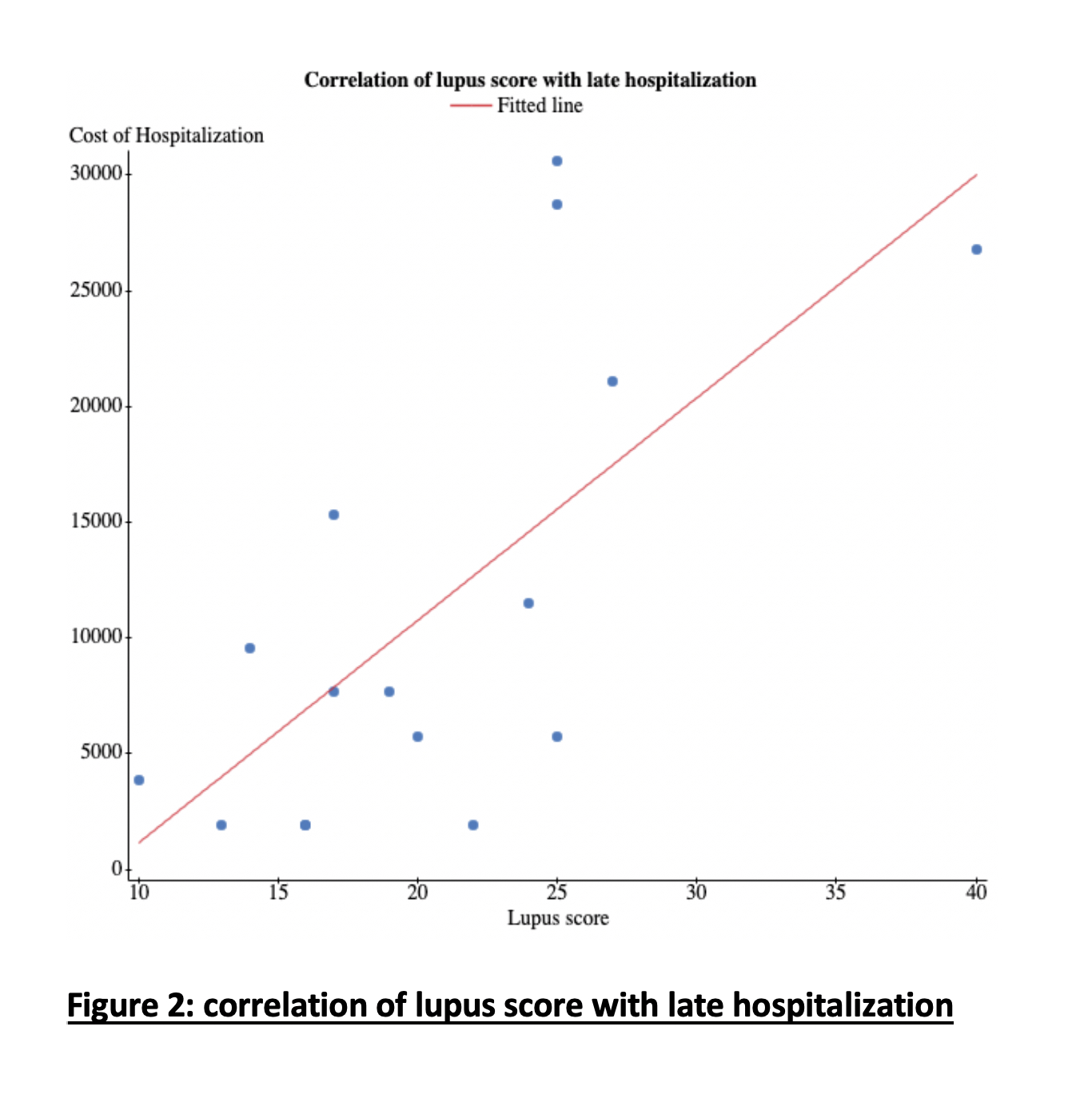 Figure 2: Correlation of Lupus Score with late hospitalization
Figure 2: Correlation of Lupus Score with late hospitalization
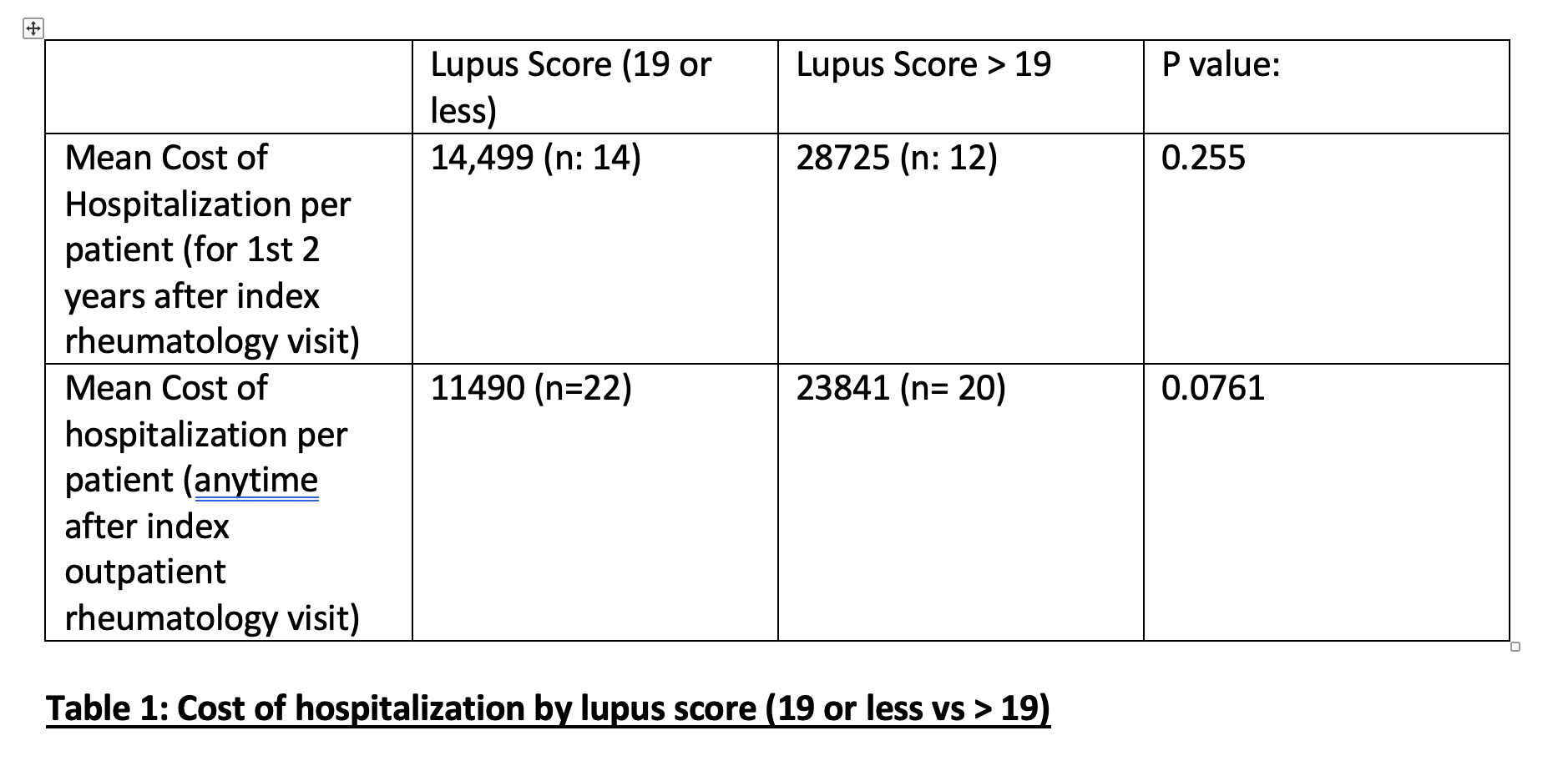 Table 1:Cost of Hospitalization by Lupus score (19 or less vs > 19)
Table 1:Cost of Hospitalization by Lupus score (19 or less vs > 19)
To cite this abstract in AMA style:
Suman S, Batool A, Keller J, Roberts W. 2019 Lupus Classification Criteria Score Predicting Cost of Future Hospitalizations [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/2019-lupus-classification-criteria-score-predicting-cost-of-future-hospitalizations/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/2019-lupus-classification-criteria-score-predicting-cost-of-future-hospitalizations/
