Session Information
Date: Sunday, November 8, 2020
Title: Epidemiology & Public Health Poster III: Inflammatory Rheumatic Disease
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Streptococcus pneumoniae, Herpes zoster, and influenza infections are common and potentially preventable causes of morbidity and mortality. Vaccinations have been shown to reduce infection rates. Unfortunately, some patients are not offered or refuse these vaccinations. Additionally, younger patients are not eligible for pneumococcal and zoster vaccines based on the current age recommendations. In this, study we aimed to determine incidence, mortality, and national costs of hospital admissions for Streptococcus pneumoniae (Strep pneumo), Herpes Zoster, and influenza infections in patients with systemic lupus erythematosus (SLE).
Methods: Data were abstracted from the National Inpatient Sample (NIS) Database. This database is the largest collection of inpatient admission data in the USA. It is a nationally representative sample of 20% of hospitalizations from approximately 1000 hospitals. The numbers in the databases are weighted to optimize national estimates. The NIS was searched for hospitalizations in 2016 containing ICD-10 SLE codes (M32, M32.1, M32.10, M32.11, M32.12, M32.13, M32.14, M32.15, M32.19, M32.8, and M32.9) as the principal or secondary diagnosis. We further limited the SLE cohort to hospitalizations with a principal discharge diagnosis of Strep pneumo infection (ICD-10 codes J13, M00.1x, A40.3, B95.3, or G00.1), Herpes Zoster (ICD 10 codes B02), and influenza (ICD 10 codes J09 or J10). The total number of discharges, age, race, length of stay (LOS), mortality and total hospital charges were recorded.
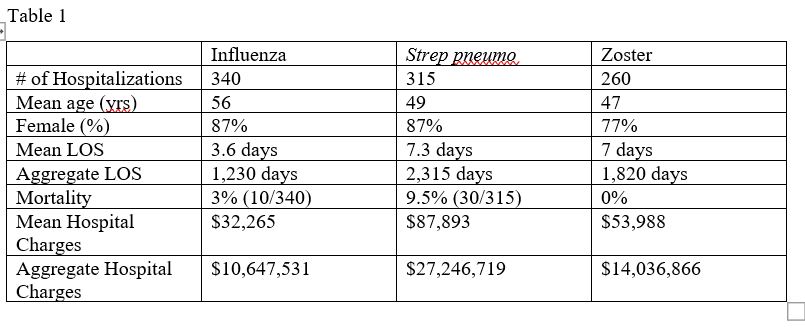
Results: Adult SLE patients had 173,765 hospitalizations in 2016. Among the SLE patients, there were 340 hospitalizations for influenza, 260 hospitalizations for zoster, and 315 hospitalizations for Streptococcus pneumoniae (see table 1).
Of the SLE patients hospitalized for influenza, mean age was 56 years, 87% were female, the mean LOS was 3.6 days, aggregate LOS 1,230 days, 3% (10/340) had in hospital mortality, the mean hospital charges were $32,265 and aggregate hospital charges were $10,647,531.
Of the SLE patients hospitalized for zoster, mean age was 47 years, 77% were female, the mean LOS was 7 days, aggregate LOS 1,820 days, 0% (0/260) had in hospital mortality, the mean hospital charges were $53,988. and aggregate hospital charges were $ 14,036,866.
Of the SLE patients hospitalized for Strep pneumo infections, the mean age was 49 years, 87% were female, the mean LOS was 7.3 days, aggregate LOS 2,315 days, 9.5% (30/315) had in hospital mortality, the mean hospital charges were $ 87,893, and the aggregate hospital charges were $27,246,719. These numbers do not account for outpatient or emergency department visits. Additionally, hospital charges are known to be higher than allowed or real charges.
Conclusion: Our analysis shows influenza, zoster, and Strep pneumo infections constituted only 0.5% of SLE hospitalizations but in-hospital mortality was high. Additionally, the economic burden of these infections was large with aggregate national hospital charges totaling over $51,931,116 and an aggregate LOS of 5,365 days. Universal vaccinations programs in SLE patients should be studied to reduce hospitalizations, cost, morbidity, and mortality.
To cite this abstract in AMA style:
Gauto-Mariotti E, Kambhatla S, Manadan A. The Incidence, Mortality, and Economic Burden of Potentially Preventable Infections in Systemic Lupus Erythematosus Patients [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/the-incidence-mortality-and-economic-burden-of-potentially-preventable-infections-in-systemic-lupus-erythematosus-patients/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-incidence-mortality-and-economic-burden-of-potentially-preventable-infections-in-systemic-lupus-erythematosus-patients/