Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Total knee arthroplasty (TKA) is one of the most frequently performed orthopedic procedures in patients with joint cartilage destruction. Calcium pyrophosphate crystal deposition (CPPD) disease is a crystal-induced arthropathy characterized by the deposition of calcium pyrophosphate crystals in the articular and periarticular tissues that might lead to inflammatory arthritis, joint damage and the need for TKA. No prior studies exist evaluating the outcomes of CPPD patients after TKA. We aim to determine the in-hospital complications, mortality, and resource utilization following TKA in patients with and without CPPD.
Methods: We queried the US National Inpatient Sample (NIS) Database from 2009-2014 in order to identify patients who had TKA. The ICD-9 code was used to identify the patients who underwent primary TKA (81.54, V43.65), and of those, we classified the patients into two groups: (i) with ICD-9 codes defining CPPD (275.49 and 712.1–712.39) and (ii) those without any CPPD code. Data collection included patient demographics and co-morbidities. Outcomes after-TKA were in-hospital mortality, length of hospitalization, hospital charges, in-hospital complications such as surgical site infections, blood loss and need for transfusion, re-operation, thromboembolism, popliteal artery injury, peroneal nerve palsy. Associations between CPPD and specific morbidity were evaluated with chi-square tests. Wilcoxon rank-sum tests were used for continuous variables.
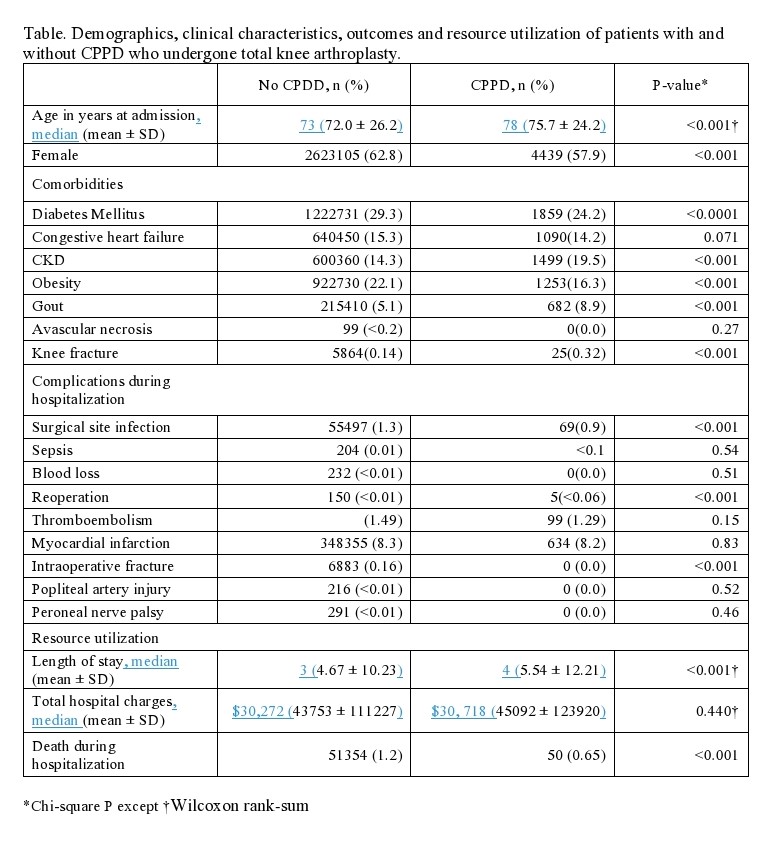
Results: Among the 4,180,274 (adjusted for sampling weight) patients who have undergone TKA during the 7-year period (2009-2014), 7660 (0.18%) had CPPD, with a median age of 73 years and 57.9% were females (Table). Compared with patients without CPPD, patients with CPPD patients were more likely to be older (median age78 vs 73 years; p< 0.0001). Co-morbidities that were more frequent among CPPD patients included chronic kidney disease, gout and knee fracture. Regarding postoperative complications, the need for re-operation was significantly more common in CPPD patients (p < 0.0001). Further, TKA in CPPD patients was associated with prolonged median length of stay than those without CPPD (4 vs 3 days; p < 0.0001), although the median total charges were higher in the CPPD group, this finding was not statistically significant ($30,718 vs $30,272; p=0.44). The in-hospital mortality was lower in the CPPD patients (0.65 vs 1.2; p< 0.001).
Conclusion: To our knowledge, this the first study demonstrating that patients with CPPD patients who had undergone TKA were more likely to be older than those without CPPD, had increased length of stay; however, the in-hospital mortality was lower. These findings merit further study.
To cite this abstract in AMA style:
Parperis K, Hadi M, Bhattarai B. Outcomes and Resource Utilization After Total Knee Arthroplasty in Calcium Pyrophosphate Crystal Deposition Disease Patients: Insights from the National Inpatient Sample Database [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/outcomes-and-resource-utilization-after-total-knee-arthroplasty-in-calcium-pyrophosphate-crystal-deposition-disease-patients-insights-from-the-national-inpatient-sample-database/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/outcomes-and-resource-utilization-after-total-knee-arthroplasty-in-calcium-pyrophosphate-crystal-deposition-disease-patients-insights-from-the-national-inpatient-sample-database/