Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: PROMIS® (Patient-Reported Outcome Measurement Information System) is a set of person-centered measures that evaluates and monitors the physical, emotional, and social aspects of health. PROMIS® measures have been used to assess health-related quality of life (HRQoL) in patients with rheumatic diseases1 and cut-points of severity in impairments have been identified for specific domains (like physical function). These measures have not been carefully evaluated in patients with persistent antiphospholipid antibodies (aPL) or with antiphospholipid syndrome (APS).
Methods: At an academic medical center, patients (n = 78) with persistent aPL seen in the rheumatology clinic prospectively completed PROMIS® Physical Function (PF) Short Form 10A v2.0, Cognitive Function (CF) Short Form 8A, and self-perceived pain intensity (PI, the scale of 1-10, with 10 being the most pain). Of the 78 patients, 51 had primary APS, 17 had secondary APS, and 10 had persistent aPL without a history of thrombotic event or pregnancy loss. Data regarding serologies and clinical manifestations associated with APS were captured; also, medications taken for mental health, pain, or seizures were recorded. Groups were compared by unpaired t-tests or one-way ANOVA; correlations were tested by Pearson’s method.
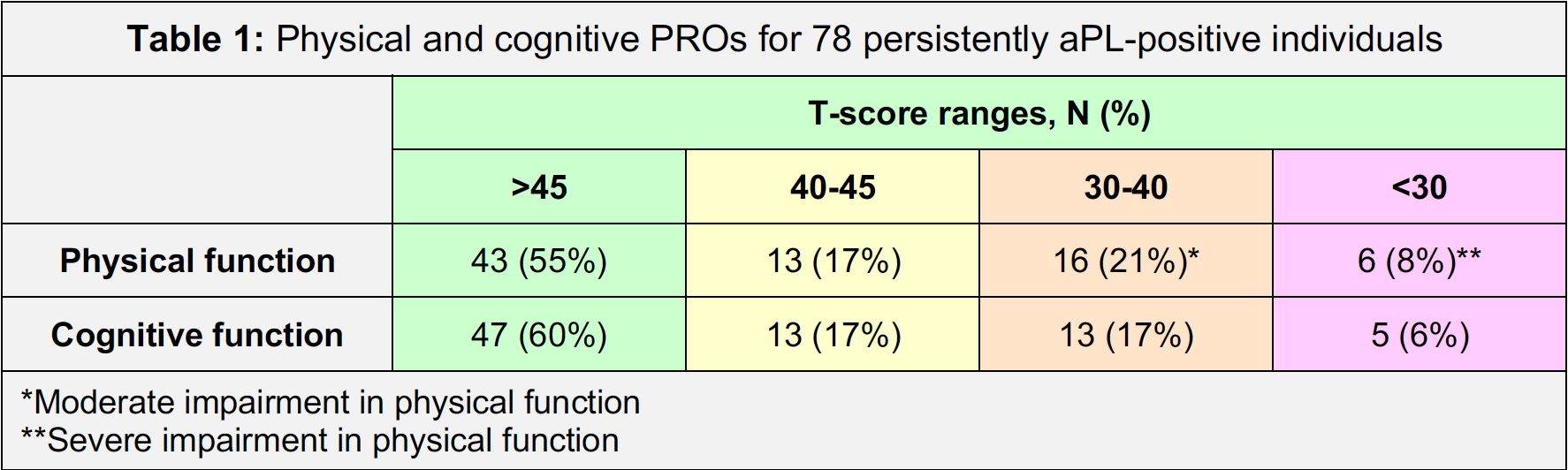
Results: For the general United States population, the T-score average is standardized at 50 ± 10 for PF and CF. For the 78 patients studied here, the average T-scores for PF and CF were 45.0 ± 9.8 and 47.5 ± 10.9, respectively; the average score for PI was 3.2 ± 2.6. Patients who endorsed more impairment on one measure endorsed more impairment on another measure (PF vs. CF, r=0.51, p< 0.0001; PF vs. PI, r=-0.55, p< 0.0001; and CF vs. PI, r=-0.33, p=0.004). About a third of the patients endorsed moderate to severe impairment in PF (Table 1). A quarter of the patients had a T-score of < 40 for CF. While clinical markers of disease (specific aPL, previous thrombotic events, etc.) did not predict PROMIS® scores, several general health and lifestyle factors (especially sedentary lifestyle) were predictive of impairments in PF and CF (Table 2). The use of medications for mental health or pain was associated with more endorsed impairments in PF and CF (Table 3).
Conclusion: In this single-center cohort of patients with positive aPL (most of whom have APS), a large minority of patients endorsed impairments in PF and CF. Health and lifestyle factors such as sedentary lifestyle and smoking and the use of certain medications (for mental health or pain) were associated with higher self-reported impairments in PF and CF. Future directions for this study include: (a) increasing the size of the cohort, (b) tracking these PROMIS® measures over time, (c) identifying cut-points of self-reported impairment in CF in comparison with legacy measures, and (d) identifying any correlation with biomarker data.
1. Nagaraja, V., Mara, C., Khanna, P.P. et al. Establishing clinical severity for PROMIS® measures in adult patients with rheumatic diseases. Qual Life Res 27, 755–764 (2018).
To cite this abstract in AMA style:
Weiner J, Gockman K, Madison J, Zuo Y, Briceño E, Nagaraja V, Knight J. Patient-Reported Outcomes in Antiphospholipid Syndrome [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/patient-reported-outcomes-in-antiphospholipid-syndrome/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patient-reported-outcomes-in-antiphospholipid-syndrome/