Session Information
Date: Friday, November 6, 2020
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Patient satisfaction associated with disease control status among PsA patients has not been extensively studied in a real-world setting. The objective of this study was to assess the impact of PsA disease control status on patient-perceived satisfaction with treatment.
Methods: A cross-sectional survey of PsA patients recruited by rheumatologists and dermatologists was conducted in France, Germany, Italy, Spain, the UK and US. Data were collected from Jun–Aug 2018 via physician- and patient-completed forms. Physicians reported if patients were currently improving, stable, unstable or deteriorating. Unstable and deteriorating patients were grouped together for this analysis. Patients reported their satisfaction with their current treatment. Patients were compared according to disease status (improving vs. unstable/deteriorating vs. stable) using parametric and non-parametric tests. Multiple ordered logistic regression analyses examined the impact of disease status on patient-reported satisfaction with treatment. The model controlled for gender, age, Body Mass Index (BMI), current advanced treatment line, pain, body surface area affected by psoriasis (BSA), number of joints affected, total number of symptoms experienced and Charlson Comorbidity Index score.
Results: Of 2867 patients (638 US, 2229 EU), 53% of patients were stable, 36% of patients were improving and 11% of patients were unstable/deteriorating.
Patients who were improving or stable more commonly received a biologic treatment than those who were unstable/deteriorating. Those who were unstable/deteriorating had a worse clinical profile than those who were improving (Table 1). After controlling for demographic and disease characteristics and treatment status regression analysis showed that patients who were unstable/deteriorating were at a significantly increased risk of being dissatisfied with treatment. There was no observed difference between patients who were stable and improving (Table 2).
Conclusion: After controlling for demographic and disease characteristics, and treatment status, PsA patients who were unstable/deteriorating had greater odds of being dissatisfied with treatment than stable/improving patients. Patient satisfaction was associated with therapy that provides highest degree of disease control stability. Given the importance of disease control stability for patient satisfaction, physicians should prioritise therapy that will ensure patients’ disease control stability in the long term.
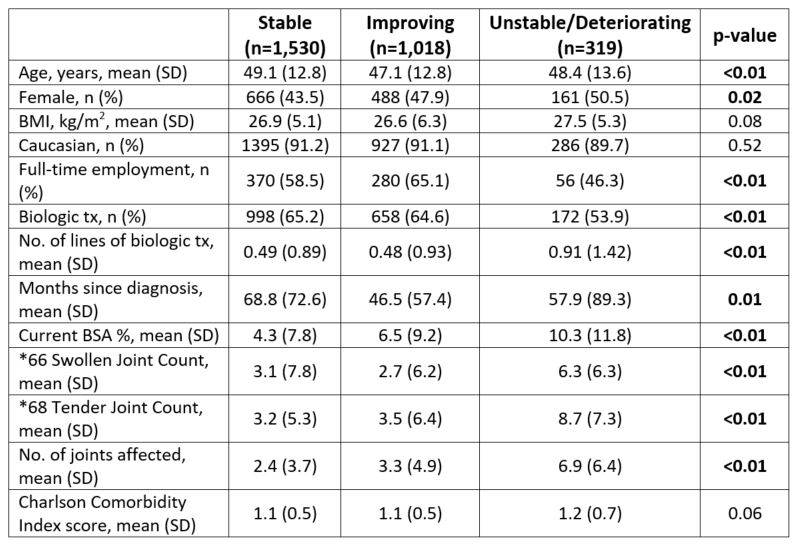 Table 1: Comparison of patient demographic and disease characteristics by physician-reported PsA disease status. *Calculated on available data: Swollen Joint Count=354, Tender Joint Count=335. Abbreviations: BMI, Body Mass Index; BSA, Body Surface Area; SD, standard deviation; tx, treatment.
Table 1: Comparison of patient demographic and disease characteristics by physician-reported PsA disease status. *Calculated on available data: Swollen Joint Count=354, Tender Joint Count=335. Abbreviations: BMI, Body Mass Index; BSA, Body Surface Area; SD, standard deviation; tx, treatment.
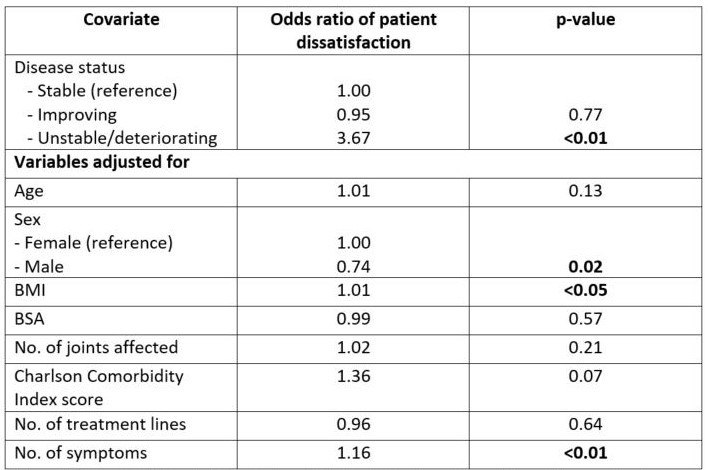 Table 2: Multivariate logistic regression model for patient satisfaction with treatment as a function of PsA disease status. Abbreviations: BMI, Body Mass Index; BSA, Body Surface Area affected by psoriasis.
Table 2: Multivariate logistic regression model for patient satisfaction with treatment as a function of PsA disease status. Abbreviations: BMI, Body Mass Index; BSA, Body Surface Area affected by psoriasis.
To cite this abstract in AMA style:
Orbai A, Holdsworth E, Baker T, Middleton-Dalby C, Shawi M, Booth N, Piercy J, Peterson S. The Impact of PsA Disease Control Status on Patient Treatment Satisfaction: Real-world Survey in US and Europe [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/the-impact-of-psa-disease-control-status-on-patient-treatment-satisfaction-real-world-survey-in-us-and-europe/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-psa-disease-control-status-on-patient-treatment-satisfaction-real-world-survey-in-us-and-europe/
