Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Infections in patients with rheumatic disease are a leading cause of morbidity and mortality. Preventive measures such as immunizations can reduce the burden of infections. In 2019 the United States experienced a surge in measles infections with significant outbreaks totaling more than 1,000 cases. Most of these outbreaks were associated with communities opposed to vaccination for varying reasons. With increased outbreaks, little attention has been given to communities at increased risk for measles secondary to limited access to care. Current guidelines for infectious disease screening prior to immune modulating therapy do not discuss measles. The Centers for Disease Control defines measles immunity as a positive titer, or evidence of two MMR vaccines, or birth prior to 1957. Seroprevalence studies of Central American countries have shown less than optimal rates of immunity to measles. We describe measles immune status in our cohort of majority underserved, Hispanic, non-U.S. born patients with rheumatic diseases.
Methods: Cross-sectional with a convenience sample of 266 patients born after 1957 who were seen in a rheumatology clinic from May 2019 to February 2020. All patients were participants in a rheumatic disease natural history study. Titer for anti-rubeola IgG was requested for each patient with their routine clinical lab draw. Immunization records were requested from primary care providers for patients whose titers were negative or equivocal. Demographic information including age, sex, place of birth, rheumatic disease diagnosis, and willingness to be vaccinated at a future visit were collected. To compare immune and non-immune groups, t tests and chi square tests were used on demographic variables where appropriate.
Results: The cohort was comprised of 86.8% women, 66.9% Hispanic ethnicity, and 52.6% from Central America or Mexico. Forty-five patients (17%) had negative or equivocal titers (Table 1), and none had records documenting prior measles immunization. Patients born in Central America or Mexico (64.4%, n=29) were more likely to be non-immune (p=0.04) than patients born elsewhere (35.6%, n=16) . Nineteen of the 45 non-immune patients (42%) were potentially eligible to receive a live vaccine. Each of these patients indicated willingness to receive the MMR vaccine at a future visit. Patients from Guatemala had the highest percentage of non-immune titers, while those from Peru had the lowest percentage non-immune titers (Figure 1).
Conclusion: Our study demonstrates susceptibility to measles in our cohort with those from Central America or Mexico more likely to be non-immune. We highlight an underserved immigrant community affected by rheumatic diseases at increased risk for morbidity and mortality related to measles outbreaks. Evidence of measles susceptibility in our cohort coupled with the finding that 42% of our non-immune patients were eligible to receive live vaccines highlights an unmet need to evaluate measles immunity in rheumatology patients prior to immune-modulating therapy particularly in underserved populations. Clinicians can avoid missed opportunities to reduce infection risk in these at-risk communities by integrating immunizations into daily practice.
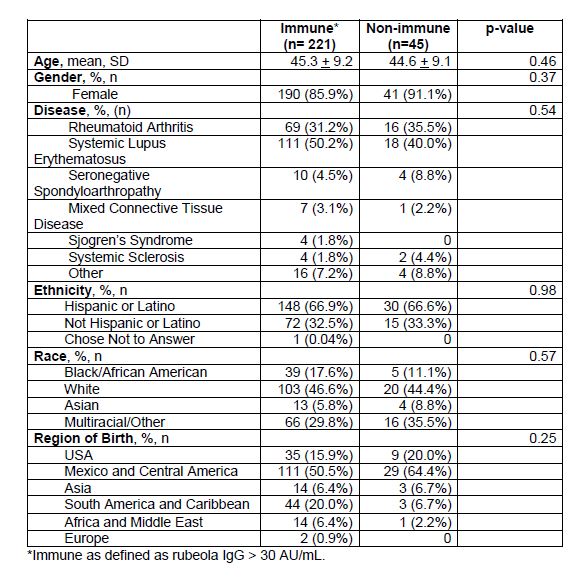 Table 1: Demographics of Patients Tested for Measles Immune Status
Table 1: Demographics of Patients Tested for Measles Immune Status
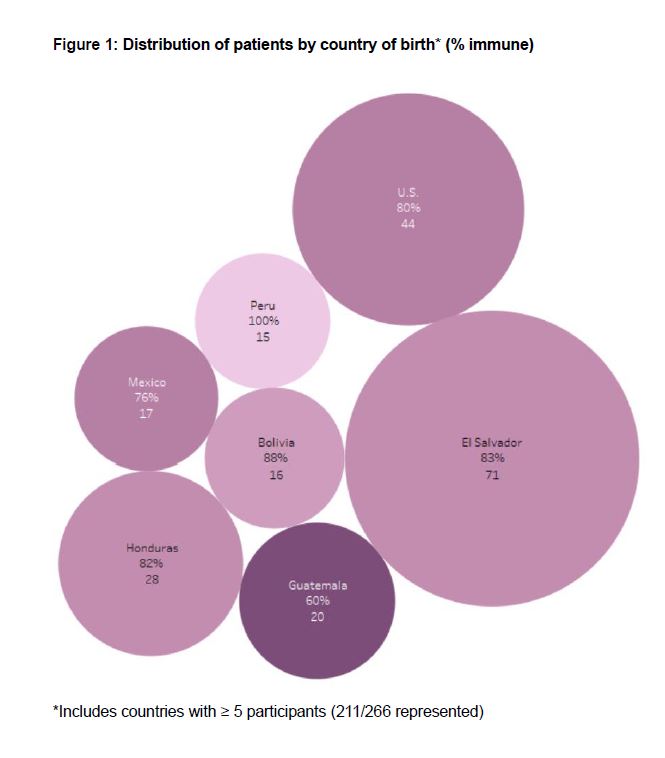 Figure 1: Distribution of patients by country of birth* (% immune)
Figure 1: Distribution of patients by country of birth* (% immune)
To cite this abstract in AMA style:
Fike A, Amarnani A, Ruiz-Perdomo Y, Hasni S, Ward M, Katz J. Increased Susceptibility to Measles in Patients from Central America and Mexico in a U.S. Rheumatology Clinic [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/increased-susceptibility-to-measles-in-patients-from-central-america-and-mexico-in-a-u-s-rheumatology-clinic/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-susceptibility-to-measles-in-patients-from-central-america-and-mexico-in-a-u-s-rheumatology-clinic/
