Session Information
The 2020 Pediatric Rheumatology Symposium, originally scheduled for April 29 – May 2, was postponed due to COVID-19; therefore, abstracts were not presented as scheduled.
Date: Friday, May 1, 2020
Title: Poster Session 2
Session Type: ACR Abstract Session
Session Time: 5:00PM-6:00PM
Background/Purpose: Kawasaki disease (KD) is a well described vasculitis of childhood that is the leading cause of acquired heart disease in developed countries. Kawasaki disease shock syndrome (KDSS) has been described in a limited number of small single center cohorts and case reports but the incidence and prognosis is poorly understood. Here we aim to add to the existing body of knowledge by describing patients with the diagnoses of KD and shock at our institution.
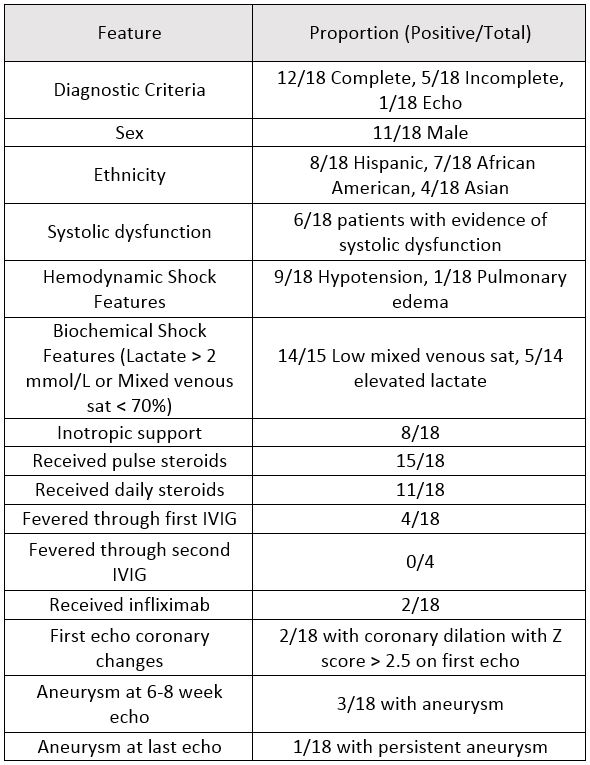
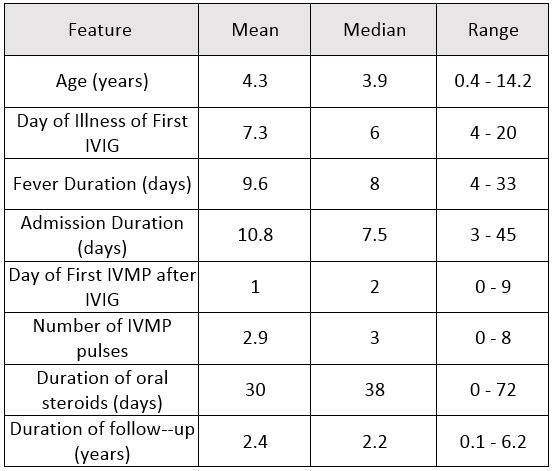
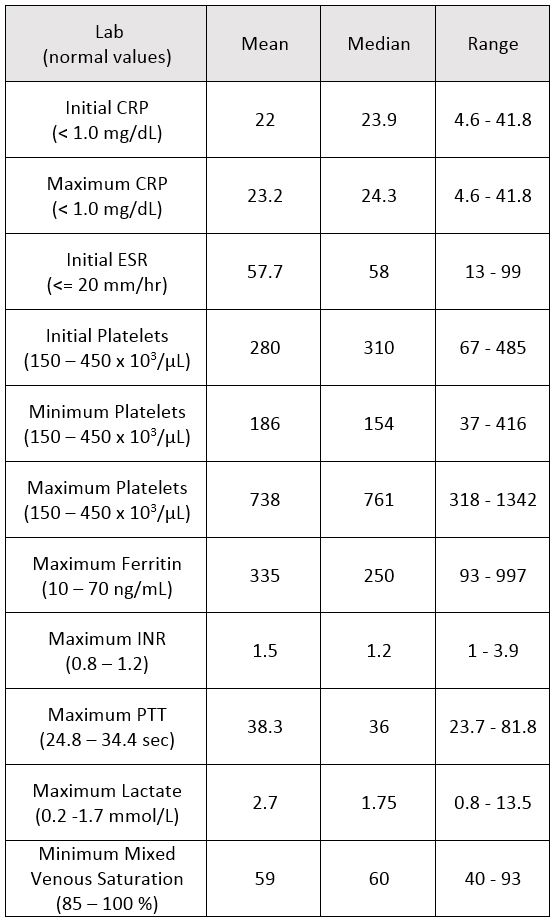
Methods: With approval from the Baylor College of Medicine IRB, all pediatric intensive care unit (PICU) admissions with a rheumatology consult were identified between March 2012 and February 2016 (269 total) and retrospectively reviewed for a diagnosis. Thirty patients were diagnosed with KD; 27 patients had the specific diagnosis of KDSS. The diagnosis of shock was confirmed by the combination of clinical concern requiring PICU admission and objective evidence defined by hypotension for age or laboratory evidence of impaired perfusion (lactate > 2.0 mmol/L or mixed venous sat < 70%). Five of these 30 patients were excluded due to timing of hypotension occurring during IVIG infusion. Seven of the 30 did not have objective evidence of shock. The 18 remaining patients’ charts were reviewed for the features presented in tables and results. During this time, 486 total KD diagnoses were identified using SlicerDicer. Results: The patients described in our cohort were predominantly African American (39%) and Hispanic (44%) and mostly male (61%). The mean age was 4.3 years and the mean duration of fever was 9.8 days. Eight of 18 (44%) patients required inotropic support for their shock with one of the patients requiring extracorporal membrane oxygenation (ECMO). The shock was mostly distributive in nature with only one patient presenting with isolated cardiac dysfunction evidenced by pulmonary edema. Six of 18 (33%) patients had platelets below 100 on admission, 11/17 (65%) had evidence of coagulopathy and 4/16 (25%) had a ferritin above 500. Fifteen of 18 (83%) received pulse dose steroids and 11/18 (61%) received daily steroids. Steroids were given an average of 2 days after the IVIG. Four of 18 (22%) patients fevered through the first IVIG and had fever resolution after a second IVIG. Two of 18 received infliximab after fever resolution. Six of 18 (33%) of the patients had evidence of systolic dysfunction on initial echo and 2/18 (11%) had evidence of coronary dilation with z-score > 2.5 on initial echo. On the 6-8 week echo, 3/18 (17%) had evidence of aneurysm with z-score > 2.5 but this had resolved by recent follow-up in all but one patient (6%).
Conclusion: All of our KDSS patients had good coronary outcomes except one patient who required ECMO and had 33 days of fever. In general the patients received early treatment with pulse steroids but there were 3 patients who received no steroids. The steroids were not typically given immediately as distinguishing KDSS from sepsis without blood cultures can be challenging. The frequency of shock in KD was 4% at our institution. We suspect that our outcomes are different from previously published data due to the use of early pulse dose steroids. The true utility of steroids is limited by the small cohort size and variety of dosing regimens.
To cite this abstract in AMA style:
Bray M, Rammel J, Ramirez A, Sexson K, Lam F, Muscal E, De Guzman M. Kawasaki Disease Shock Syndrome: A Single Center Cohort [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 4). https://acrabstracts.org/abstract/kawasaki-disease-shock-syndrome-a-single-center-cohort/. Accessed .« Back to 2020 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/kawasaki-disease-shock-syndrome-a-single-center-cohort/