Session Information
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Up to 83% of patients with SLE are nonadherent to hydroxychloroquine (HCQ) which results in a 36% higher risk of renal failure, and 8-fold higher risk of premature death. Therefore, clinicians must address HCQ nonadherence. Our recent meta-analysis reported three times higher odds of low HCQ blood levels in SLE patients who self-report HCQ nonadherence. Results suggest that when asked, most patients accurately report HCQ adherence. Despite this, one study reported that patients were never asked about medication nonadherence during 200 recorded rheumatology visits at 4 centers. Barriers to addressing nonadherence include limited time and expertise in using lengthy gold-standard self-report tools (14+ items). Therefore, we aimed to develop a tool to assess nonadherence, categorize specific adherence barriers, and guide clinicians to prepare an adherence plan with individual SLE patients.
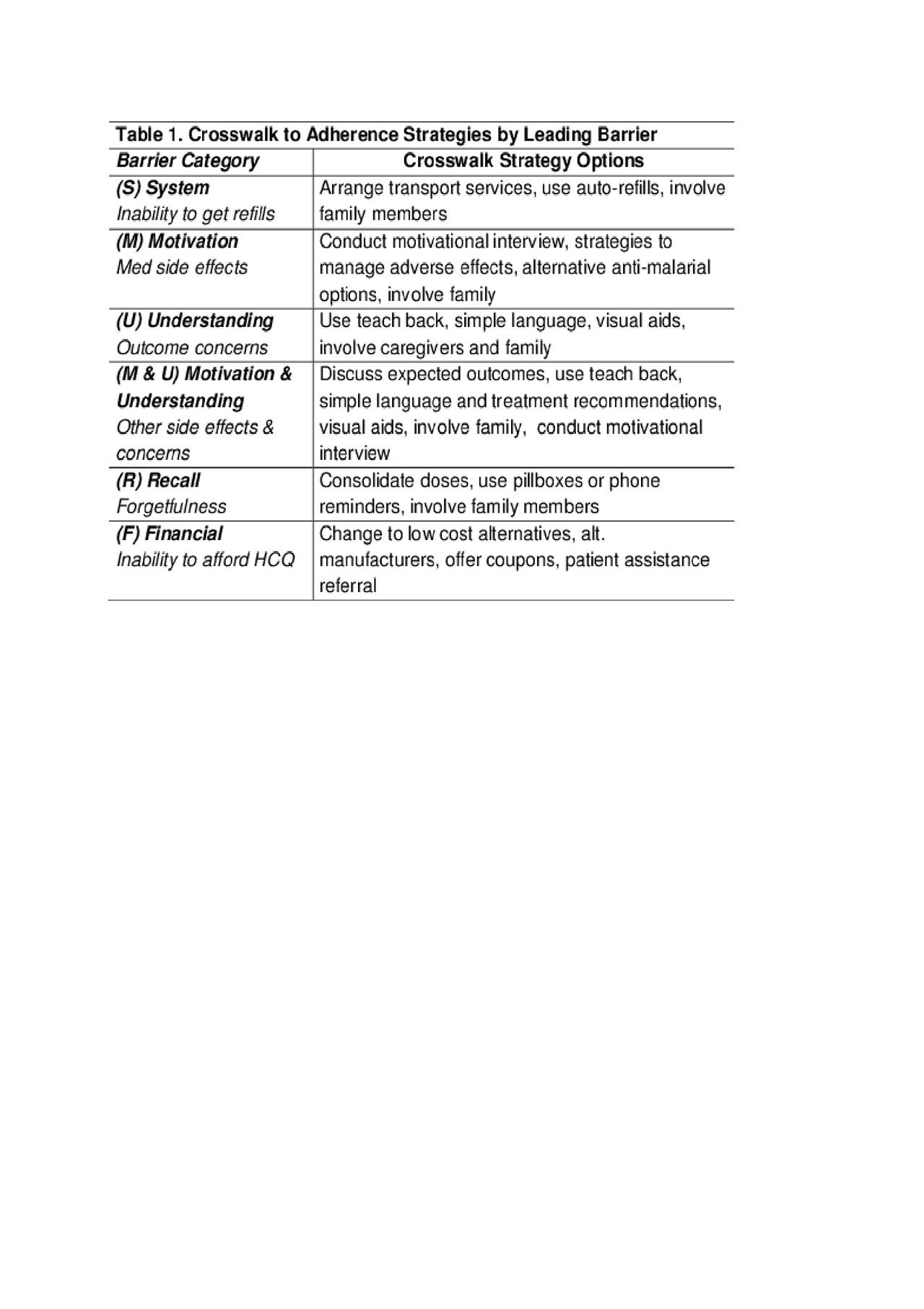
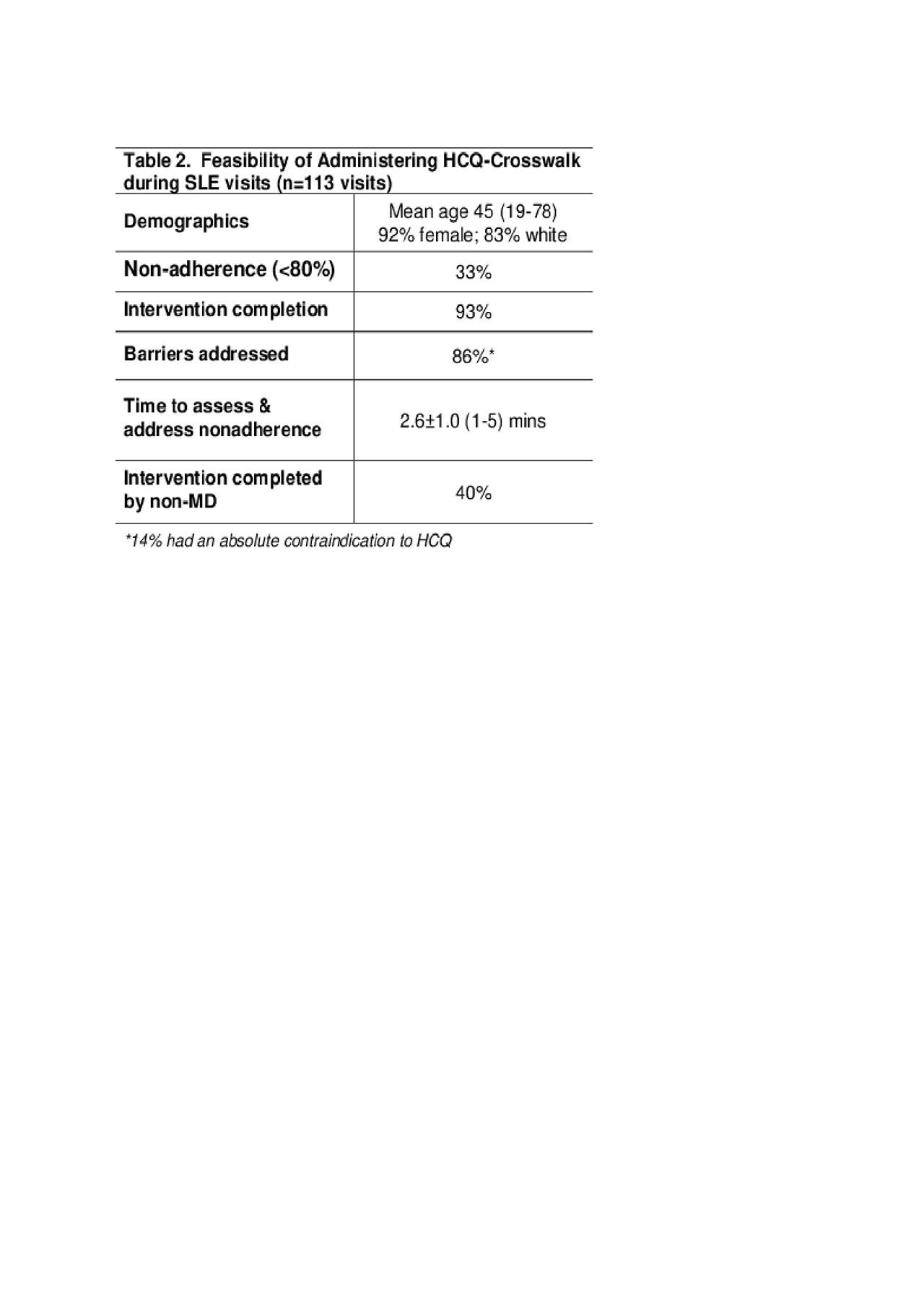
Methods: We implemented a 26-week single center study to test the feasibility of administering our adapted seven-item HCQ Adherence Tailoring Crosswalk (HCQ-Crosswalk) intervention in all consecutive SLE visits (n =113). The intervention was based on key domains of two gold-standard adherence tools (MASRI & BMQ). The first item, a visual-analogue adherence scale, was completed by SLE patients. Those who reported nonadherence (adherence < 80%) on the first item were prompted to complete the next six questions to identify their key adherence barrier(s). Upon identifying 1-2 key adherence barrier categories, clinicians were directed to the crosswalk to adherence strategies (Table 1) which were discussed with patients to tailor an individual adherence plan. To assess the tool’s feasibility, we calculated the percentage of visits completing the intervention, the mean time spent, the percentage of barriers addressed, and proportion completed by a non-MD (e.g. pharmacy student).
Results: Nonadherence was identified at 33% of 113 consecutive visits among 65 SLE patients. Nonadherence rates were comparable to published rates using a gold-standard tool (33% vs 51%, p 0.08). The HCQ-Crosswalk intervention was completed in 93% of visits. Patients reported Motivation & Understanding as the key barrier (43%), which included the fear of side effects and lack of knowledge on long-term benefits of HCQ (Figure 1). Other commonly reported barriers included forgetfulness (Recall) and inability to afford medications (Financial). Using this intervention, we addressed 86% of barriers within 2.6±1 mins and 40% of the discussions were completed by a non-MD (Table 2).
Conclusion: The HCQ-Crosswalk is a feasible intervention to assess and address nonadherence in under 3 minutes. Future work will aim to validate HCQ-Crosswalk intervention versus gold-standard tools and to examine its role in improving HCQ adherence in SLE.
To cite this abstract in AMA style:
Garg S, Chewning B, Hansen K, Martin B, Bartels C. Improving SLE Care by Enhancing Medication Adherence Using a Tailored Clinic Intervention: HCQ-Crosswalk [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/improving-sle-care-by-enhancing-medication-adherence-using-a-tailored-clinic-intervention-hcq-crosswalk/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improving-sle-care-by-enhancing-medication-adherence-using-a-tailored-clinic-intervention-hcq-crosswalk/