Session Information
Date: Tuesday, November 12, 2019
Title: 5T098: Orthopedics, Low Back Pain & Rehabilitation (2798–2803)
Session Type: ACR/ARP Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Meniscal tear is an independent risk factor of structural progression in OA; Arthroscopic partial meniscectomy (APM) is also associated with progression, though it is unclear if APM confers additional risk beyond that of the underlying meniscal tear. The goal of this study was to evaluate changes in knee MRI findings over 60 months in patients with meniscal tear and OA treated with either APM (and postop physical therapy (PT)) or with PT alone as a part of a multicenter RCT.
Methods: We used data from an RCT of APM and PT vs. PT alone (denoted in this abstract as APM vs. PT) for patients ≥ 45 years old with knee pain, meniscal tear on MRI, and OA changes on radiograph or MRI. Patients were excluded from this analysis if they were randomized to but did not receive APM, crossed over to APM > 6 months from randomization, or if they had no MRIs. We performed as-treated analysis: subjects who crossed over from PT to APM within 6 months from randomization were analyzed in the APM group.
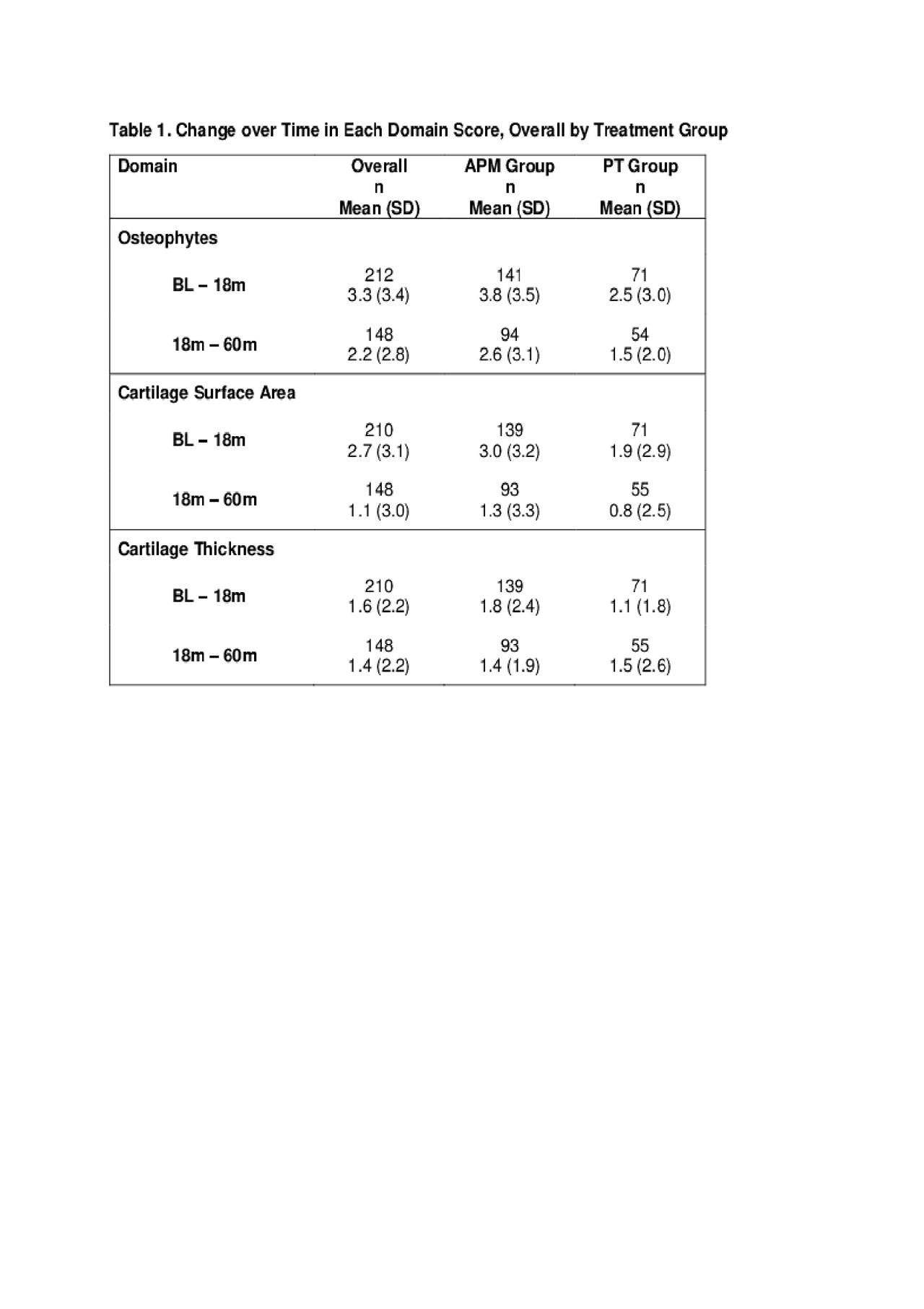
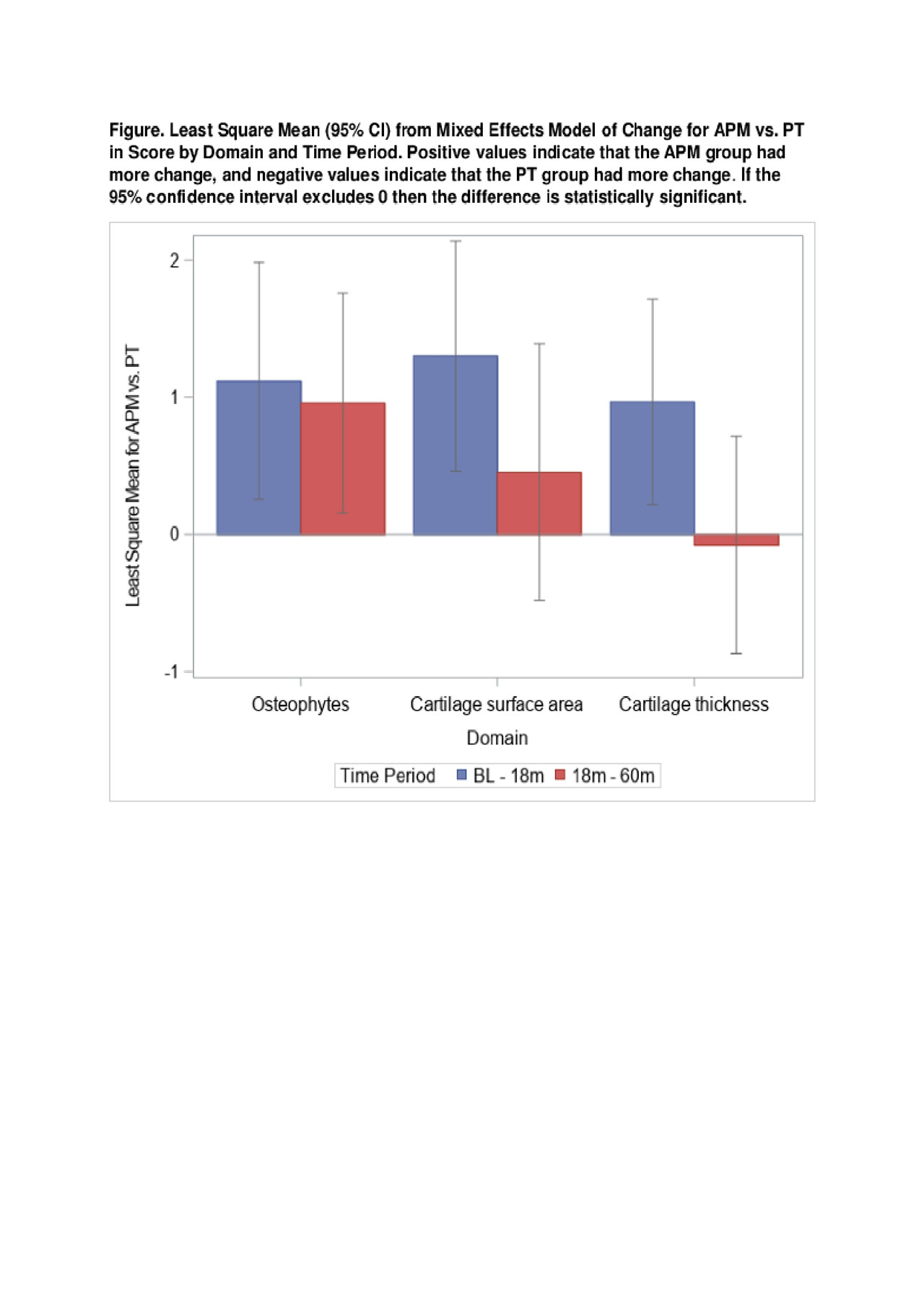
Baseline (BL), 18-month (18m), and 60-month (60m) MRIs were read using the MRI OA Knee Score (MOAKS), which assesses damage in several joint features including osteophyte, cartilage surface area, and cartilage thickness. Each feature was scored ordinally from 0 – 3, (higher is worse) in each of 14 subregions (SR) for cartilage and 12 for osteophytes. We summed the scores from all SRs within the osteophyte, cartilage surface area and cartilage thickness domains. We used a linear mixed effects model to assess the relationship between the APM and PT groups and the changes in damage scores within each domain for two time intervals: BL-18m and 18m-60m.
Results: Of 351 randomized subjects, we excluded 10 randomized to but not undergoing APM, 14 randomized to PT who crossed over after 6m and 32 with no MRI. The analytic cohort included 295 subjects with mean age 58 (SD 7) years and mean baseline KOOS pain (0-100, 100 worst) 47 (SD 16). 193 (65%) received APM and 102 (35%) received PT. The groups were balanced on BL demographic and clinical characteristics. 285 (97%) subjects had MRI at BL 221 (75%) at 18m and 165 (56%) at 60m.
Descriptive statistics on change in both time periods are presented in the Table. Both treatment groups worsened in all domains for both time periods, with more worsening over BL – 18m than 18m – 60m. The Figure displays the difference in change in score for each domain for APM vs. PT, from the mixed effects model. Worsening in osteophyte score was significantly greater in the APM group vs. the PT group for both time periods. Change in both cartilage surface area and cartilage thickness scores were significantly different between the groups for the BL – 18m period, but not the 18m – 60m period.
Conclusion: In subjects with underlying meniscal tear, APM was associated with greater worsening in cartilage surface area, cartilage thickness, and osteophytes over 18m post randomization, and greater worsening in osteophytes, but not in cartilage scores, in the subsequent 42 months. Future work will consider missing not at random imputation for subjects undergoing TKR, examine outcomes from an intention to treat perspective, and determine the magnitude of change in structure that is associated with clinically meaningful changes in symptoms.
To cite this abstract in AMA style:
Shrestha S, Katz J, Losina E, Collins J. Five Year Structural Changes in Patients with Meniscal Tear and Osteoarthritis from an RCT of Arthroscopic Partial Meniscectomy vs. Physical Therapy [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/five-year-structural-changes-in-patients-with-meniscal-tear-and-osteoarthritis-from-an-rct-of-arthroscopic-partial-meniscectomy-vs-physical-therapy/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/five-year-structural-changes-in-patients-with-meniscal-tear-and-osteoarthritis-from-an-rct-of-arthroscopic-partial-meniscectomy-vs-physical-therapy/