Session Information
Date: Tuesday, November 12, 2019
Title: Pediatric Rheumatology – ePoster III: Systemic JIA, Fever, & Vasculitis – ARP
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Uveitis is a heterogenous group of ocular inflammatory diseases. Underlying disease and treatment can lead to poor quality of life (QOL), depression, and increased health care costs. Our aim is to evaluate overall QOL, vision related QOL, anxiety and depression in a cohort of children with non-infectious uveitis at the Cincinnati Children’s Hospital Medical Center.
Methods: Patients and parents completed questionnaires within two weeks of the ophthalmic evaluation which included: Pediatric Quality of Life Inventory (PedsQL) for overall QOL, Effects of Youngsters’ Eyesight on Quality of Life (EYE-Q) for uveitis-specific QOL and function, and the Revised Children’s Anxiety and Depression Scale (RCADS) for anxiety and depression. PedsQL scores range from 0-100 and EYE-Q ranges 0-2. Higher scores indicate better overall and vision related QOL. RCADS score of >65 indicates clinically meaningful anxiety or depression. We compared children’s questionnaire scores using medians and interquartile range by diagnosis, gender, race, use of topical drops, use of systemic medications, presence of ocular complications, and uveitis activity using Wilcoxon rank sum tests (SAS software).
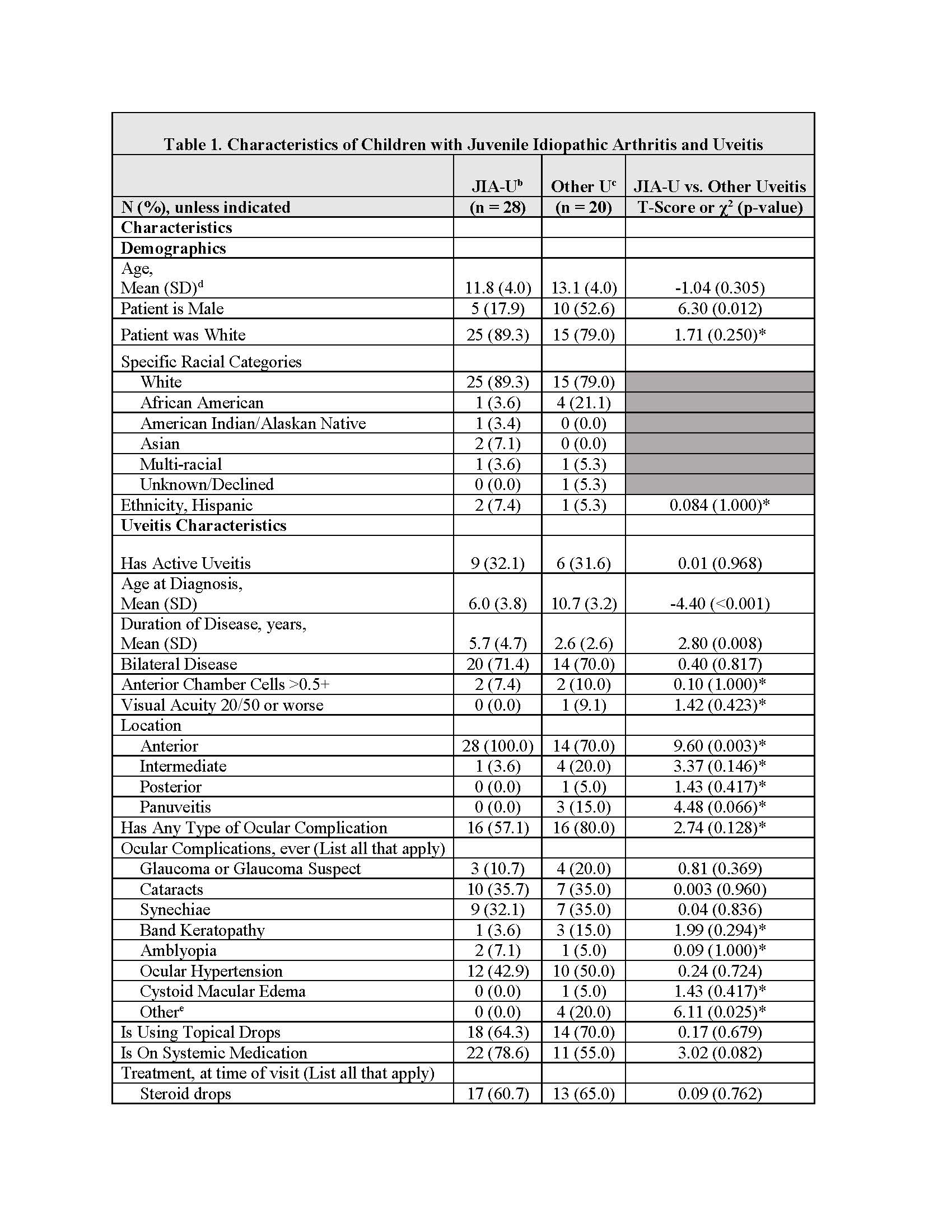
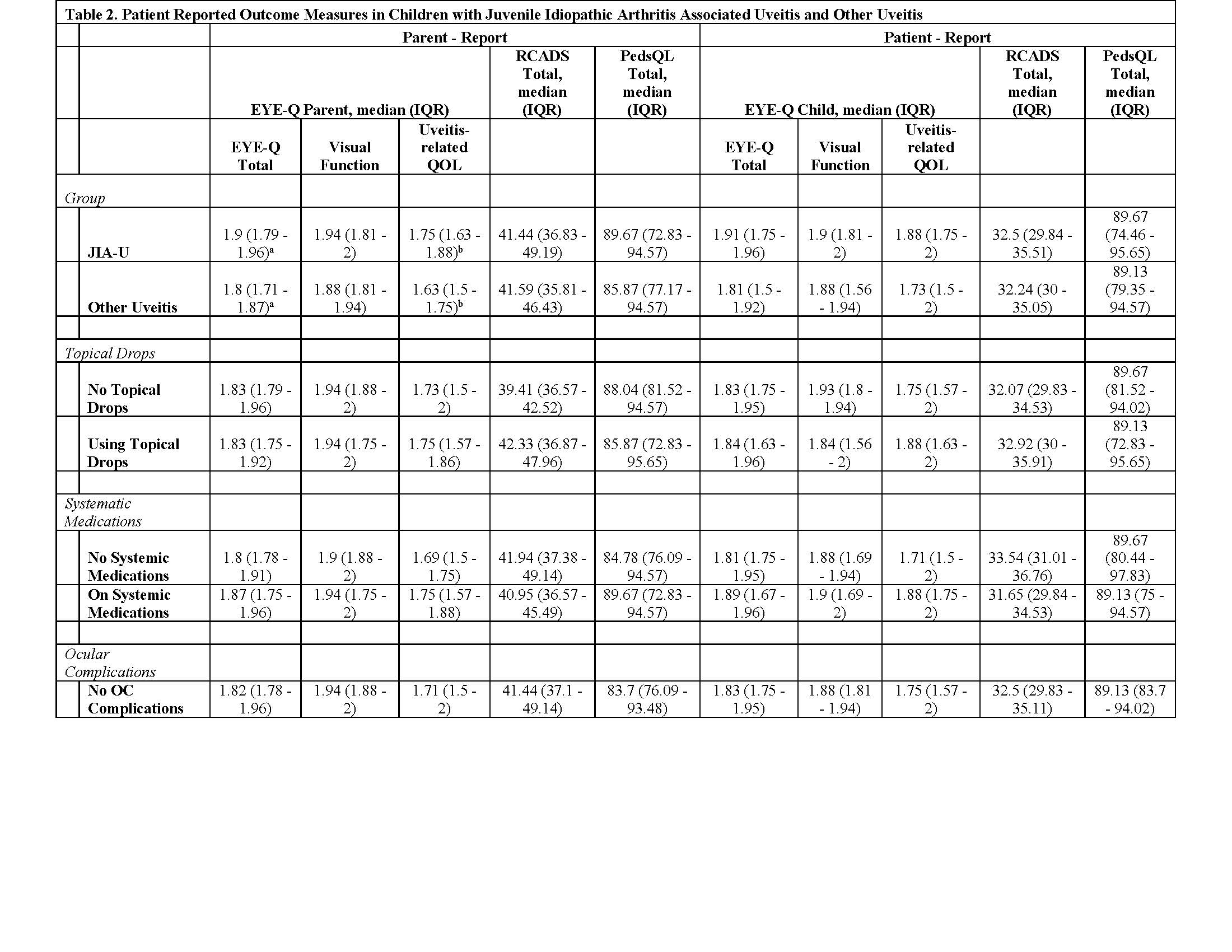
Results: Forty-eight patients were included: 28 JIA-associated uveitis (JIA-U) and 20 non-JIA-U (Other U). Children with JIA-U were primarily female (82% vs. 50%, p = 0.012), white (89% vs 75%, p = 0.012), younger at uveitis diagnosis (6 vs 10 p< 0.001), have a longer mean duration of disease (5.7 vs 2.6 years, p=0.008), and had anterior uveitis (100% vs 70%, p=0.003). (Table 1). The most common ocular complications were ocular hypertension (46%), cataract (35 %), and posterior synechiae (33%) formation. Topical medications were commonly used at last follow up (~60%), with more JIA-U patients requiring systemic immunosuppressive therapy (79% vs 55%, p=0.082). Parent and patients with JIA-U and Other U reported similar median scores on the EYE-Q, PedsQL and RCADS (Table 2). No differences were observed in QOL metrics based on topical or systemic medication use, ocular complications or uveitis activity. Although females had worse RCADS scores for both the parent (female 43.0 vs male 36.7, p< 0.05) and patient (female 33.6 vs male 30.1, p< 0.05) questionnaires, this was not clinically relevant. There was a trend towards worse uveitis related QOL in non-white patients and those with Other-U.
Conclusion: We report on the clinical characteristics, QOL and functioning of children with uveitis. Our results suggest there may be differences in QOL and function related to sex, race, and uveitis diagnosis. Larger and more diverse cohorts with varied uveitis, visual impairment and disease activity are needed to better understand the impact of uveitis and treatment on a child and family’s QOL and function.
To cite this abstract in AMA style:
Shantha J, Cassedy A, McDonald J, Hennard T, Mwase N, Yeh S, Angeles-Han S. Baseline Characteristics and Quality of Life Metrics in Non-Infectious Uveitis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/baseline-characteristics-and-quality-of-life-metrics-in-non-infectious-uveitis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/baseline-characteristics-and-quality-of-life-metrics-in-non-infectious-uveitis/