Session Information
Date: Tuesday, November 12, 2019
Title: Vasculitis – Non-ANCA-Associated & Related Disorders Poster III: Giant Cell Arteritis
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: It has been historically difficult to develop effective diagnostic strategies and criteria in giant cell arteritis (GCA). While temporal artery biopsy was previously thought of as a diagnostic standard, there has been increasing recognition of so-called ‘biopsy negative’ GCA. As such, the disease has become increasingly challenging to accurately investigate and diagnose. MRI of the scalp arteries (MRISA) has been demonstrated to be more sensitive than temporal artery biopsy, but it’s utility in the diagnosis of ‘clinical GCA’ is thus far unknown.
Methods: This analysis considered a retrospective cohort of 324 patients who had been previously referred to a rheumatologist for evaluation of possible GCA. The clinical information of 171 of these patients was made available from a previous clinical trial; the remaining 153 were consented for participation in a prospective GCA diagnostic database. A clinical diagnosis, regardless of agreement with American College of Rheumatology (ACR) criteria or biopsy, was used as the gold standard. Data concerning clinical features, inflammatory markers, imaging, and biopsy results were extracted for analysis. Best subset forward selection was used to create a multivariable logistic regression model to predict the diagnosis of GCA. Using this model, disease probabilities were calculated and the positive/negative predictive value (PPV/NPV) of MRISA in the diagnosis of clinical GCA was determined.
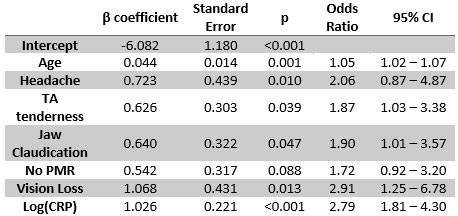
Results: As seen in table 1, univariate analysis demonstrated that those diagnosed with clinical GCA were older, more likely to have jaw claudication or vision loss, and had higher ESR and/or CRP than those without the diagnosis. An abnormal MRISA was strongly associated with the diagnosis of GCA (OR 19.82, 95% CI 10.5-37.41). Multivariable logistic regression demonstrated that increasing age, the presence of headache, temporal artery tenderness, jaw claudication, vision loss, log(CRP), and the lack of symptoms of PMR were all predictive of the diagnosis of GCA with an area under the receiver-operator curve of 0.774, 95% CI 0.719 – 0.829 (table 2). When a calculated probability of 25% or greater was considered a positive diagnosis, the model was 91.1% sensitive and 46.2% specific for the diagnosis of GCA; at 50% or greater it was 48.2% and 85.4% respectively. This compared to 54.6% and 66.0% using the 1990 ACR criteria. MRISA was found to have 64.7% sensitivity and 91.5% specificity for the clinical diagnosis of GCA. For those determined to be disease negative using the 25% cut-off, a negative MRISA was found to have an 93.5% NPV to rule out GCA; the 50% cut-off was found to have 80.9% NPV (see figure 1).
Conclusion: Multivariable logistic regression was able to fairly model the clinical diagnosis of GCA. MRISA was found to be less sensitive and more specific than previously reported in other studies in the diagnosis of biopsy positive GCA patients; this likely reflects that within this cohort the diagnosis was contaminated by MRISA being used to direct the diagnosis. Regardless, given the high NPV in those of low to medium pre-test probability of GCA, MRISA can assist in ruling out the diagnosis of GCA and avoid temporal artery biopsy.
** denotes median and interquartile range.
Receiver-Operator Characteristic = 0.774.
To cite this abstract in AMA style:
Junek M, Hu A, Beattie K, Legault K, Garner S, Rebello R, Khalidi N. Rationalizing the Use of MRI of the Scalp Arteries in the Diagnosis of Giant Cell Arteritis Through Multivariable Predictive Modelling [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/rationalizing-the-use-of-mri-of-the-scalp-arteries-in-the-diagnosis-of-giant-cell-arteritis-through-multivariable-predictive-modelling/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rationalizing-the-use-of-mri-of-the-scalp-arteries-in-the-diagnosis-of-giant-cell-arteritis-through-multivariable-predictive-modelling/