Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Rapidly Progressive Glomerulonephritis (RPGN) is characterized clinically by a rapid and severe decline in kidney function. Thus, this entity may lead to an end stage renal disease, with kidney transplantation. RPGN is classificated in three groups: a) Type I or associated to anti-glomerular basement membrane antibodies (RPGN-GBMa), b) Type II or associated to immunocomplexes (RGPN-immunocomplexes), and c) Type III or pauci-immune (RPGN-pauci-immune). Besides, RPGN can be primary, without extra-renal involvement (RPGN-renal-limited), or secondary to systemic autoimmune disorders (RPGN-SAD), infectious diseases or drugs. Kidney transplantation in RPGN-SAD may be associated to a worse outcome.
In a series of 42 patients with first transplantation due to RPGN our aim was to assess a) clinical features of the three types of RPGN, b) comparison of post-transplant survival and graft survival between these three types.
Methods: We study three groups of patients according to renal biopsy: a) RPGN-GBMa (n = 11), b) RPGN-immunocomplexes (n = 2) and c) RPGN-pauci-immune (n=29).
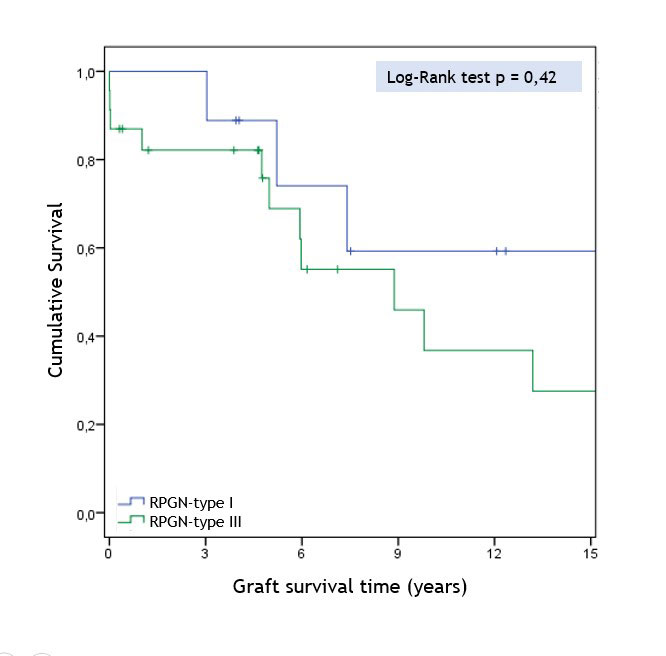
All these patients were transplanted in a single reference University Hospital. The main outcome variables were a) graft survival up to 15 years and patient survival up to 30 years and b) evolution of renal function (serum creatinine and proteinuria) in the first 5 years of follow-up. Cumulative survival rates after transplantation were estimated by the Kaplan-Meier method and compared between groups using the log-rank test. Kruskal-Wallis test was used to compare quantitative variables and chi2/Fisher’s exact test for qualitative variables.
Results: We included a total of 42 patients with renal transplant due to RPGN, with a mean age at diagnosis of 44.87±17.01 years (48.53±17.45 at the time of the transplant). No significant differences at baseline were observed between the three RPGN groups regarding sex, age and cardiovascular risk factors. Renal biopsy had been performed in the 42 patients with RPGN: type I or RPGN-GBMa (n=11, 26.2%), type II or RPGN-immunocomplexes (n=2, 4.8%) and type III or RPGN-pauci-immune (n=29, 69.0%).
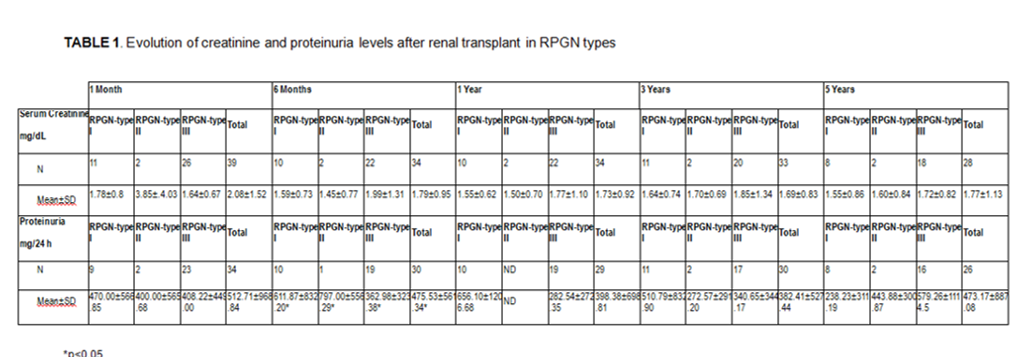
It was also reported the presence or absence of systemic autoimmune disorders (31% RPGN-SAD and 69% RPGN-renal-limited). According to the presentation and the clinical characteristics of the patients, another classification has been established: a) type I (18.2% (2) Goodpasture-syndrome), b) type II (100% renal-limited), c) type III (13.8% (4) granulomatosis with polyangiitis and 20.70% (6) microscopic polyangiitis. The evolution of serum creatinine and the proteinuria after the transplant is shown in TABLE 1. There were no significant differences between the three groups in the serum creatinine values during at 1st, 6th, 12th, 36th and 60th months post-transplant. Neither differences were found in terms of graft and patient survival between the 3 groups (Figures 1 and 2).
Conclusion: Our study shows similar graft and patient survival as well as renal outcome in renal transplant due to the three types of RPGN. Therefore, renal transplantation could be the best option for patients with end stage renal disease due to RPGN regardless of systemic manifestations.
To cite this abstract in AMA style:
Sanchez-Bilbao L, De Cos-Gomez M, Gonzalez-Mazon I, Atienza-Mateo B, Martín-Varillas J, Calderón-Goercke M, PRIETO- PENA D, Ruiz-San Millan J, Gonzalez-Gay M, Blanco R. Comparative Study of Renal Transplantation Due to Rapidly Progressive Glomerulonephritis (RPGN): Study of 42 Patients from a Single Tertiary Centre [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/comparative-study-of-renal-transplantation-due-to-rapidly-progressive-glomerulonephritis-rpgn-study-of-42-patients-from-a-single-tertiary-centre/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparative-study-of-renal-transplantation-due-to-rapidly-progressive-glomerulonephritis-rpgn-study-of-42-patients-from-a-single-tertiary-centre/