Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: About 30% of patients with skin psoriasis (PsO) develop psoriatic arthritis (PsA). The reasons for why only some progress to synovio-enthesial disease from skin involvement remains unknown. Genetic, environmental and clinical-demographic factors have been implicated, but are yet to be characterized in specialized, combined care centers. We aim to describe clinical phenotypes differentiating patients with PsO from those with PsA at a large, urban tertiary care PsO-PsA clinic.
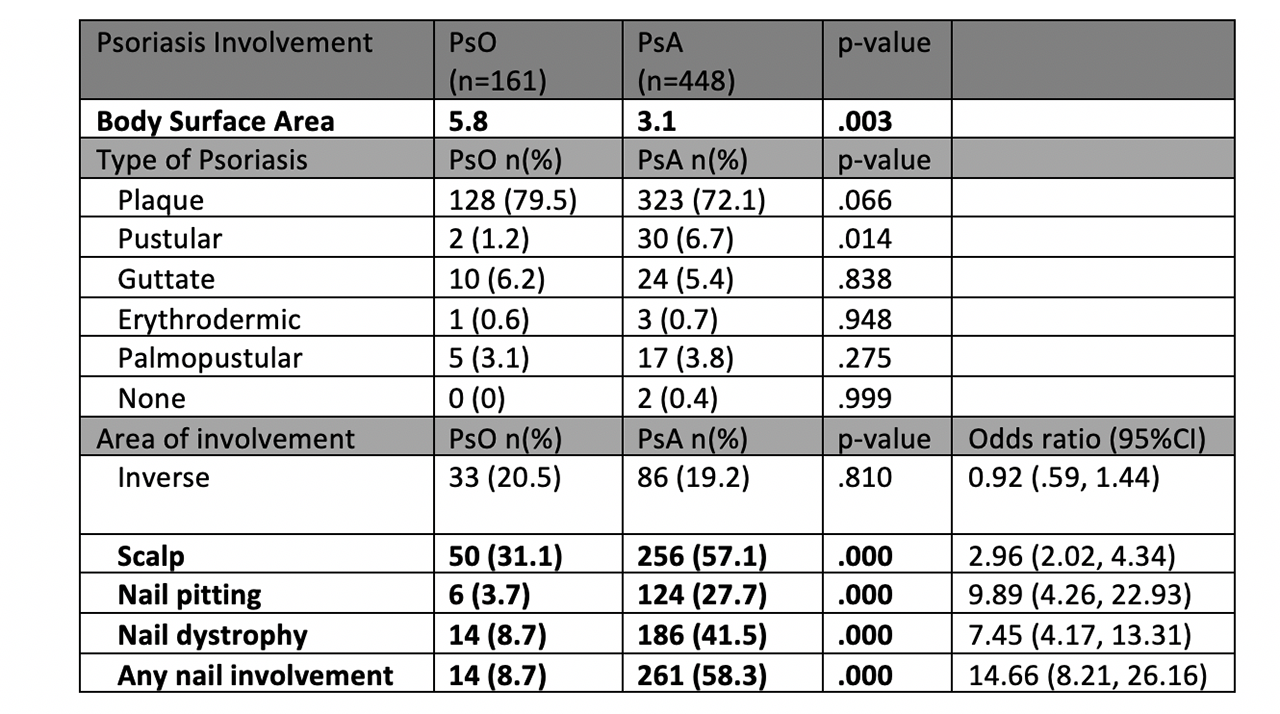
Methods: Consecutive adult patients meeting CASPAR criteria for PsA (n= 448) or with dermatologist diagnosed skin psoriasis only (n=161) were prospectively recruited at the NYU Psoriatic Arthritis Center and the NYU Psoriasis and Psoriatic Arthritis Clinic. All data was collected utilizing clinical visit notes and additional on-site questionnaires. Type of psoriasis and body surface area (BSA) was determined by dermatologists or rheumatologists specializing in psoriatic disease. Data was analyzed using statistical software SPSS using chi squared test with Yates Continuity Correction for dichotomous/categorical variables and t-test for continuous variables.
Results: Patients with PsO were more likely to be older (52.7 vs. 48.9, p=.032) and have hypertension, obesity, diabetes, and history of myocardial infarction (Figure 1). Patients with PsO had a statistically higher BSA than those with PsA (5.8% vs 3.1%, p=.003). While the type of psoriasis was similar, the site of psoriasis involvement (specifically the scalp and nail) differentiated the populations (Table 1). In PsA compared to PsO, the odds ratio of scalp involvement was 2.96 (95% Confidence Interval [CI] 2.02, 4.34) and that of nail involvement was 14.66 (95% CI 8.21, 26.16). Inverse psoriasis was not different between groups. Additionally, those with PsA were much more likely to have a first degree relative (FDR) with psoriasis compared to those with cutaneous disease alone (31.9% vs. 12.0%, p=.007) (Figure 1).
Conclusion: We report for the first time the comorbidities and psoriasis features of PsA and PsO populations in a large, combined center. We found that scalp involvement and any nail involvement was more prevalent in the PsA as compared to PsO. Only one previous study has identified scalp psoriasis[1] as a possible risk factor for progression, while previous studies looking at nail psoriasis reported much lower odds ratios[1,2]. Patients with PsA also demonstrated a higher number of FDRs with skin psoriasis, reinforcing the notion of strong heritability in PsA. The identification of risk factors for progression is of critical importance to study natural history of psoriatic disease and to inform the adequate design of prevention trials in psoriasis patients who have enriched features associated with future transition to synovio-enthesial disease.
References:
1. Wilson, F. C. et al. Incidence and clinical predictors of psoriatic arthritis in patients with psoriasis: a population-based study. Arthritis Rheum 61, 233-239, doi:10.1002/art.24172 (2009).
2. Eder, L. et al. The Incidence and Risk Factors for Psoriatic Arthritis in Patients with Psoriasis: A Prospective Cohort Study. Arthritis Rheum 68, 915-923, doi:10.1002/art.39494 (2016).
To cite this abstract in AMA style:
Haberman R, Adhikari S, Ramirez D, Lydon E, Attur M, Lovisi B, Reddy S, Neimann A, Troxel A, Scher J. Assessing Risk of PsA Progression: Results from a Combined Psoriasis-PsA Center Cohort [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/assessing-risk-of-psa-progression-results-from-a-combined-psoriasis-psa-center-cohort/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessing-risk-of-psa-progression-results-from-a-combined-psoriasis-psa-center-cohort/