Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Assessment of disease activity in psoriatic arthritis (PsA) requires evaluation of multiple aspects and can be difficult. Perception of disease activity by patient and physician is frequently discordant (1). The aim of our study was to evaluate factors associated with persistence of disease activity evaluated by patients yet considered in remission by their rheumatologist.
Methods: We performed a transversal monocentric study. PsA patients were included if they met the CASPAR criteria and if they were considered in remission by their rheumatologist. Demographic data, characteristics of the disease, treatments were collected. Disease activity was evaluated by several scores: Disease Activity Score (DAS28-CRP), Simple Disease Activity Index (SDAI), Clinical Disease Activity Index (CDAI), Disease Activity in Psoriatic Arthritis (DAPSA), Minimal Disease Activity (MDA), modified Boolean remission criteria for PsA. We collected multiple Patient’s Reported Outcomes (PROs): Psoriatic Arthritis Impact of Disease (PsAID), Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), Bath Ankylosing Spondylitis Functional Index (BASFI), Health Assessment Questionnaire (HAQ), Dermatology Life Quality Index (DLQI), Beck Depression Inventory (BDI), Fibromyalgia Rapid Screening Tool (FiRST), Pain Catastrophizing Scale (PCS). Discordance was defined by a difference between patient’s and rheumatologist’s global assessment ≥30/100 on a Visual Analogue Scale (VAS). Univariate and multivariate analyses were performed to evaluate factors associated with the presence of discordance.
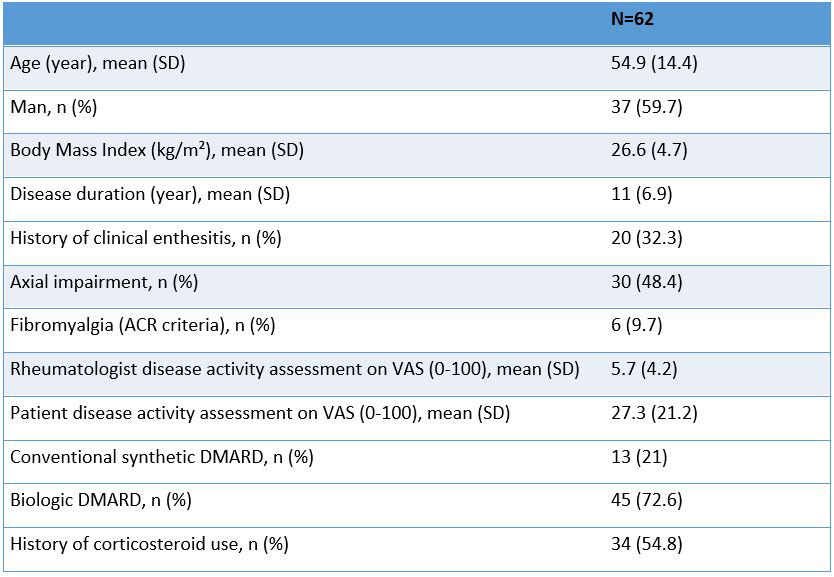
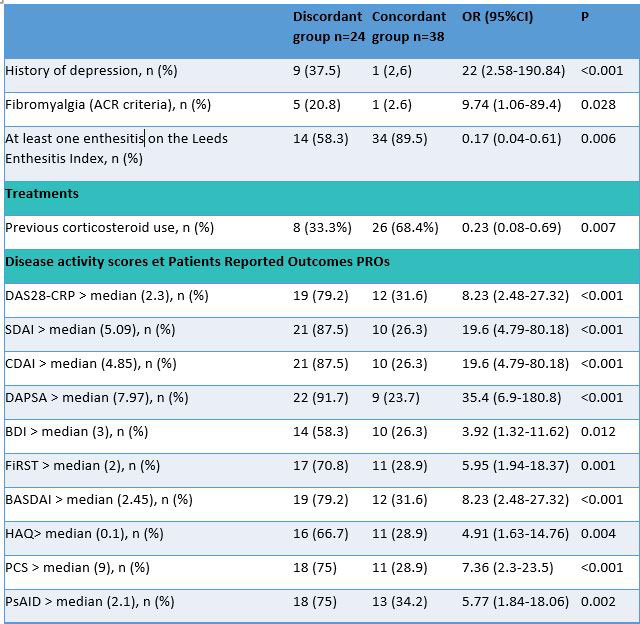
Results: 62 PsA patients were included. 40.3 % were women and the mean (SD) age was 55 (14) years (Table 1). 61% patients were in remission (rheumatologist definition) for more than 12 months and 19% for less than 3 months. 50% met MDA, 63% DAS28-CRP < 2,6, 39% SDAI and CDAI remission, 27% DAPSA remission, and 8% Booleans remission criteria. 39% had a discordant disease activity assessment from their rheumatologist. In univariate analysis, factors associated with discordance were a history of depression, an associated fibromyalgia, a history of clinical enthesitis and a history of corticosteroid use (Table 2). All disease activity scores and PROs were higher in discordant group and were associated with discordance in univariate analysis. In multivariate analysis, discordance was associated with no previous corticosteroid use (OR 24.5 (95%CI 2.9-203.7), p=0.003), a higher BDI scale (OR 1.4 (95%CI 1.1-1.8) by supplementary point, p=0.017) and a higher DAPSA score (OR 1.5 (95%CI 1.2-2), p< 0.001) by supplementary point.
Conclusion: In this PsA cohort, discordance between patient and rheumatologist is very common. Discordance in assessment of disease activity was associated with no previous corticosteroid use, probably reflecting a less severe disease, presence of depressive symptoms and an increase of DAPSA, reflecting a more active disease.
To cite this abstract in AMA style:
Moly M, Lukas C, Morel J, Combe B, Mouterde G. Factors Associated with Discordance Between Patient and Rheumatologist Assessment of Disease Activity in Psoriatic Arthritis Considered in Remission [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/factors-associated-with-discordance-between-patient-and-rheumatologist-assessment-of-disease-activity-in-psoriatic-arthritis-considered-in-remission/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-associated-with-discordance-between-patient-and-rheumatologist-assessment-of-disease-activity-in-psoriatic-arthritis-considered-in-remission/