Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: pSS is characterized by lymphocytic infiltration of salivary gland epithelial cells (SGEC). This infiltrate is made of T (TL) and B (BL) lymphocytes. SGEC are now known to be active players of the pathogenesis of the disease. Here we aimed to focus on the crosstalk between SGEC and TL in pSS and on the impact of IL7 on this process given the role of IL7 on TL biology.
Methods: IL-7 serum level was assessed in 372 pSS patients and 73 paired controls. Primary cultures of salivary gland epithelial cells (SGEC) from patients and controls were stimulated by Poly I:C 30 ng/ml, IFN-α 600UI/ml, IFN-γ 5ng/ml and IFN-λ (IL-28) 25ng/ml for 72 hours. IL-7 secretion was tested in culture supernatant (SN) by ELISA and by quantitative RT-PCR. Four-day and eight-day co-cultures (allogenic and then autologous) between LT and SGEC were performed in presence of Poly IC and anti-CD3/anti-CD28 and anti IL7-R (OSE-127, 10 µg/ml) or control isotype. TL survival and activation were assessed by FACS. Last, explants from minor salivary gland biopsies (MSGB) from 9 pSS patients and 3 controls were cultured for 4 days in presence of anti IL7-R (OSE-127, 10 µg/ml) or control isotype. Transcriptomic analysis from the biopsies (explants and cells in the SN) was studied by Nanostring (Immunology panel_v2).
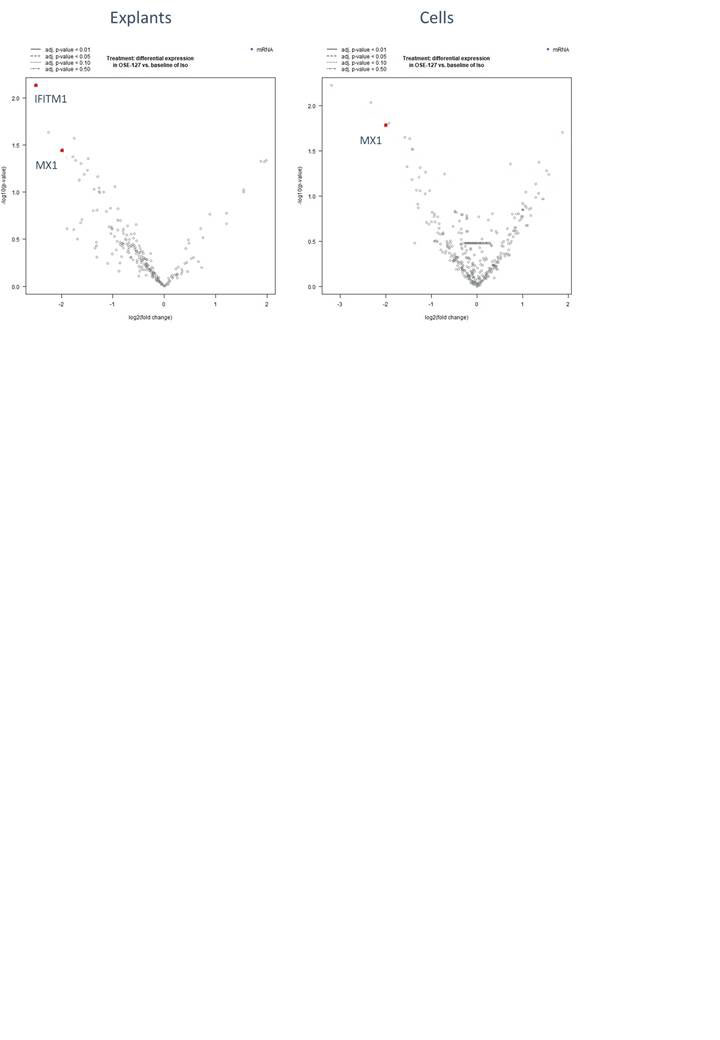
Results: pSS patients had higher serum IL-7 levels than controls: 7.56 ng/ml ± 8.52 (mean ± SD) versus 4.86 ng/ml ± 5.59; p< 0.0001. SGEC stimulation with Poly I:C, IFN-α, -γ and -λ induced IL-7 protein secretion in the supernatant (p=0.002, p=0.004, p=0.007, p=0.004 respectively). IL-7 expression was confirmed by quantitative RT-PCR. Allogenic co-culture lead to increased activation of TL as assessed by increased HLA-DR expression and this was partially inhibited by adding OSE-127 in the co-culture. This activation was not observed in autologous co-cultures. Co-cultures of SGECs with either allogenic or autologous TL showed that TL survival was increased by co-culture and this effect was not abolished by inhibiting IL7 signaling with OSE-127. Lastly, analysis of the mRNA signature from MSGB explants from pSS patients revealed that inhibition of IL7 signaling by OSE-127 lead to a decreased of IFN signature as assessed by decreased expression of IFITM1 and Mx-1 both in the explants and in the cells in the SN (Figure).
Conclusion: This study shows that IL7, a key TL cytokine, is increased in pSS and is locally produced by SGEC after PolyI:C and IFNs stimulation. SGEC are likely to have a feeder effect allowing survival of TL but it seems to be independent of IL7. However and interestingly, IL7 signaling may participate to the IFN signature observed in different glandular cellular sub-types in pSS, as demonstrated by decreased IFN signature after IL7-R inhibition both in the explant and in the cellular SN.
To cite this abstract in AMA style:
Nocturne G, Pascaud J, Rivière E, Virone A, Dupré A, Gauttier V, Poirier N, Mariette X. In Primary Sjogren’s Syndrome (pSS) IL7 Promotes the Crosstalk Between T Lymphocytes and Salivary Gland Epithelial Cells and Participates to IFN Signature [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/in-primary-sjogrens-syndrome-pss-il7-promotes-the-crosstalk-between-t-lymphocytes-and-salivary-gland-epithelial-cells-and-participates-to-ifn-signature/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/in-primary-sjogrens-syndrome-pss-il7-promotes-the-crosstalk-between-t-lymphocytes-and-salivary-gland-epithelial-cells-and-participates-to-ifn-signature/