Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Autoantibodies and chronic systemic inflammation experienced in rheumatoid arthritis (RA) increases the risk of cardiovascular disease (CVD). This systematic literature review (SLR) aimed to characterize the available evidence with respect to the effect of DMARDs on cardiovascular outcomes in patients with RA with and without history of CVD.
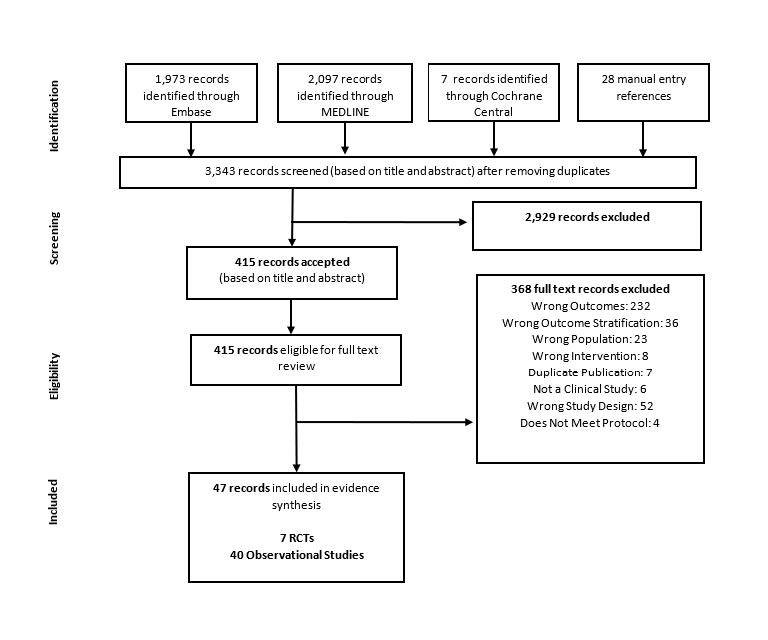
Methods: A SLR was conducted by searching MEDLINE, Embase, and Cochrane CENTRAL databases (inception to Jan. 2019) supplemented by a search in conference proceedings from ACR and EULAR (2017 to 2019), and US and European clinical trial registries (Jan. 2005 to Jan. 2018). Studies eligible for inclusion were observational studies and randomized controlled trials (RCTs) investigating adult patients with RA treated with biologic and non-biologic DMARDs and reporting cardiovascular events including major adverse cardiac events (MACE), other cardiovascular event composites, myocardial infarction (MI), stroke, and heart failure.
Results: As described in Figure 1, the SLR yielded 47 eligible publications, including 7 RCTs, 6 prospective observational, and 34 retrospective observational studies. Baseline rates of CVD (0%-83%) or history of cardiovascular events (0%-80.1%) varied between studies with six studies entirely excluding patients with cardiovascular comorbidities.
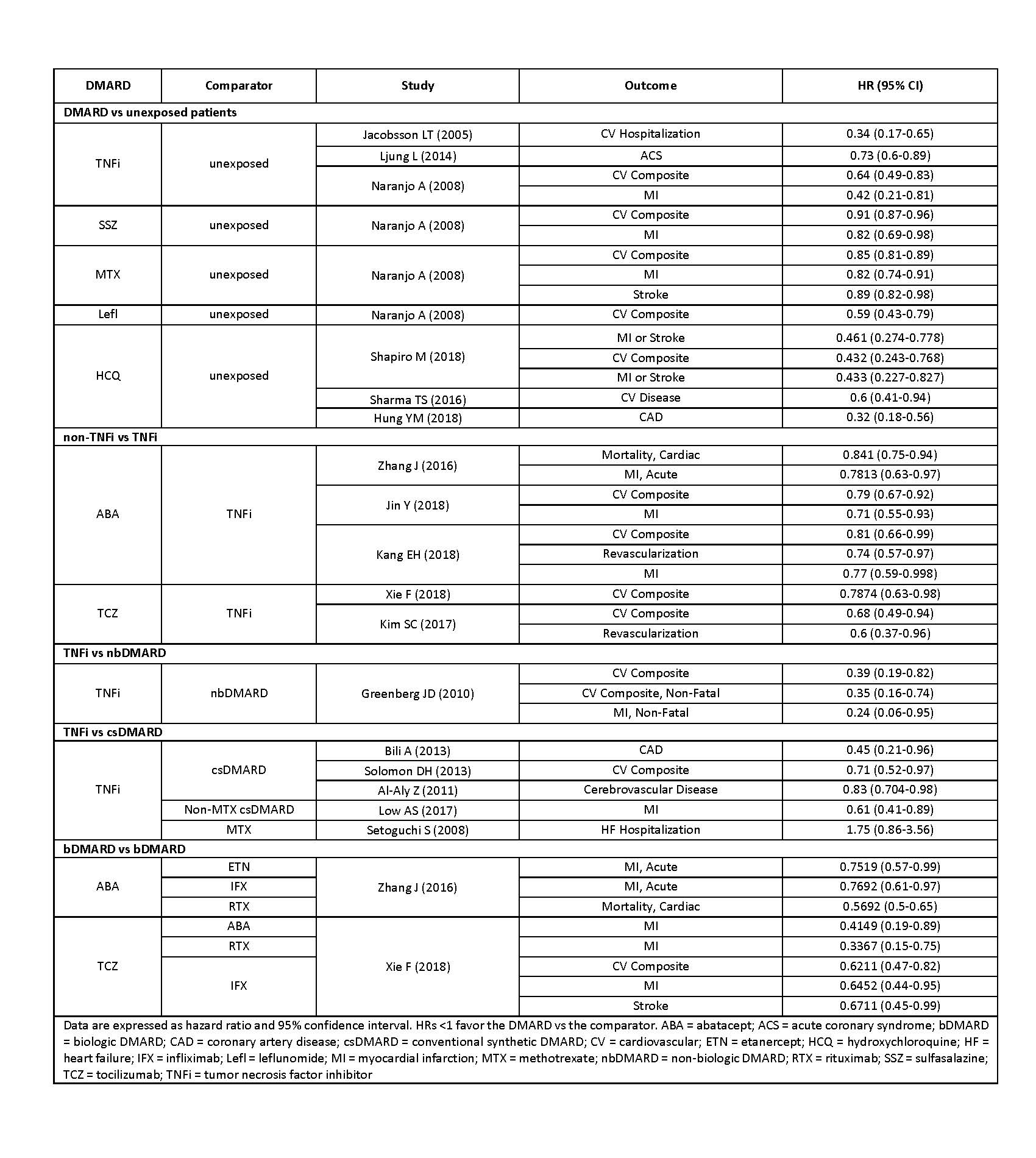
The most commonly reported outcomes were cardiovascular event composites (MACE or other) and MI (Table 1). Incidence rates (per 1000 person-years) for any cardiovascular event composite ranged from 3.1-30.7 for csDMARDs, 2.93-35.8 for TNF inhibitors (TNFi) and 3.7-23.8 for non-TNFi. The rate of MI ranged from 2.38-10.4 for csDMARDs, 0.51-9.3 for TNFi and 2-8.43 for non-TNFi. Rates were heterogenous across studies, likely due to differences in cardiovascular characteristics. One study found a five-fold increase in cardiovascular outcomes for patients with a history of CVD, HR 5.302.
Twenty studies reported statistically significant differences between DMARDs for a variety of cardiovascular outcomes (Table 2). Compared to unexposed patients, hydroxychloroquine, TNFi, sulfasalazine, leflunomide, and methotrexate significantly lowered risk of cardiovascular outcomes with HRs ranging from 0.32 (95% CI 0.18-0.56) to 0.89 (0.82-0.98). Head-to-head comparisons of DMARDs found abatacept to significantly lower cardiovascular outcomes compared to TNFi [0.71 (0.55-0.93) to 0.841 (0.75-0.94)]. Another non-TNFi biologic, rituximab, also significantly lowered risk of CV events [0.78 (0.63-0.98)]. TNFi significantly lowered outcome rates compared to non-biologic DMARDs [0.24 (0.06-0.95) to 0.39 (0.19-0.82)] and csDMARDs [0.45 (0.21-0.96) to 0.83 (0.704-0.98)], although a single study found TNFi inferior to MTX for heart failure requiring hospitalization [1.7 (1.07-2.69)].
Conclusion: This review found the rate of cardiovascular outcomes to vary widely across studies. We found DMARDs to consistently lower the rate of cardiovascular events compared to unexposed patients. Although data is still limited, multiple studies reported that non-TNFi significantly lower cardiovascular event rates compared to TNFi.
To cite this abstract in AMA style:
Patel V, Ferri L, Han X, Mintzer L, Fazeli M. The Effect of DMARDs on Cardiovascular Outcomes in Rheumatoid Arthritis: A Systematic Literature Review [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-effect-of-dmards-on-cardiovascular-outcomes-in-rheumatoid-arthritis-a-systematic-literature-review/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-effect-of-dmards-on-cardiovascular-outcomes-in-rheumatoid-arthritis-a-systematic-literature-review/