Session Information
Date: Tuesday, November 12, 2019
Title: Epidemiology & Public Health Poster III: OA, Gout, & Other Diseases – ARP
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Pain is a hallmark of arthritis. Despite growing attention to chronic pain (CP), surprisingly little is known about its magnitude and impact among the 54.4 million US adults with arthritis. We studied two pain outcomes, CP and high impact chronic pain (HICP), among US adults age ≥18 years with a focus on those with arthritis.
Methods: We analyzed 2016/2017 data from the population-based US National Health Interview Survey (NHIS) (59, 696 participants). Arthritis was a “yes” (n=16,732) to “Have you ever been told by a doctor or other health professional that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?” We calculated crude and age-standardized prevalence of CP (pain most/all days in past 6 months) and HICP (CP that limited life or work activities on most/all days in the past 6 months) among US adults overall and by arthritis status. Then, among all US adults, we estimated the multivariable-adjusted association with prevalence ratios (PR) from logistic regression models between each pain outcome and 14 chronic conditions and 6 socio-demographic characteristics. Finally, we calculated CP and HICP prevalence among adults with arthritis across socio-demographic characteristics, health status, and comorbidities.
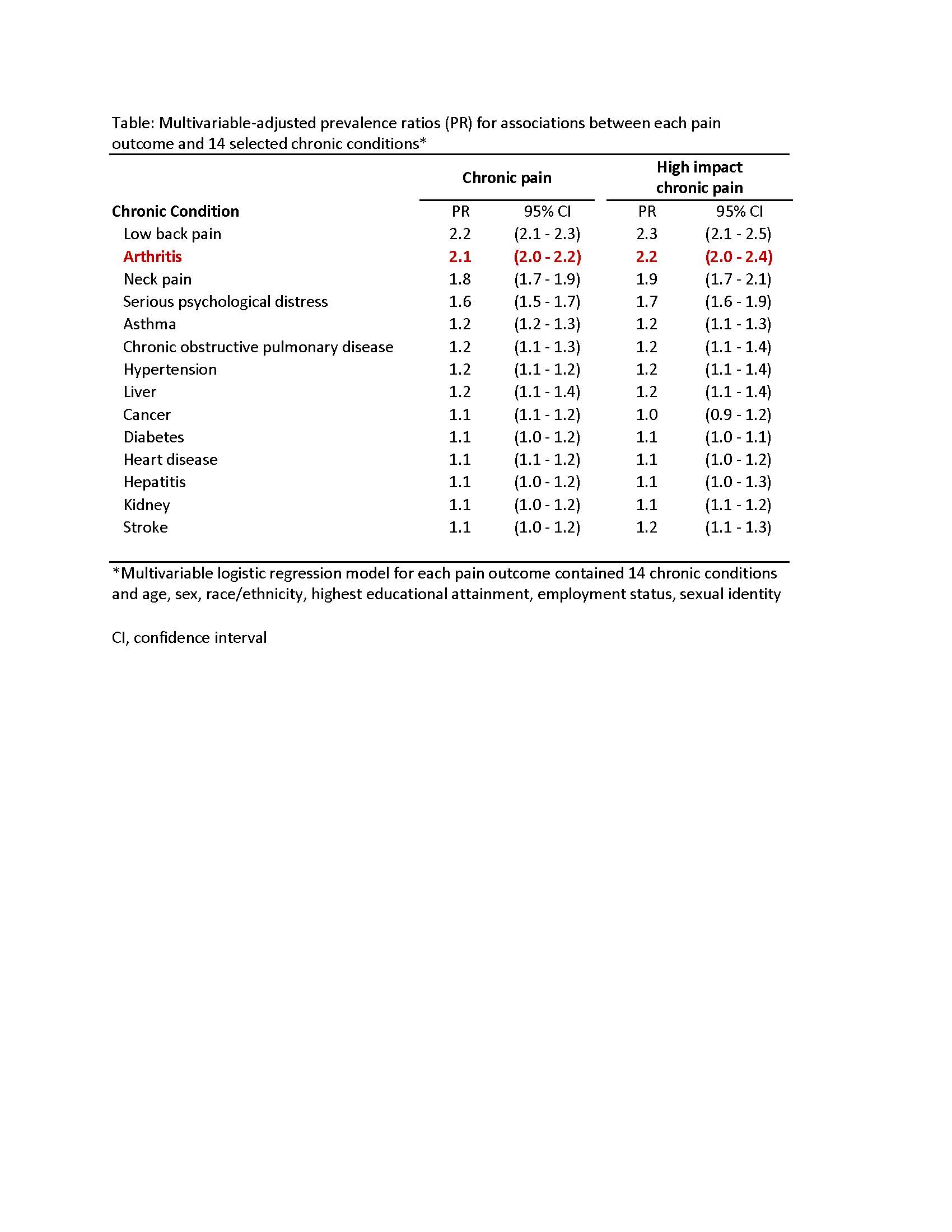
Results: Crude CP and HICP prevalence among adults with arthritis was 48.4% and 21.6%, respectively (Figure). Both CP and HICP age-standardized prevalence for adults with arthritis was higher than for US adults overall and those without arthritis, respectively (CP=48.5%, 19.2%, and 11.6%; HICP=21.4%, 7.1%, and 3.3%). In multivariable modelling, across all conditions examined, arthritis had the second strongest association with CP (PR=2.1; 95% CI=2.0-2.2) and HICP (PR=2.2; 95% CI=2.1-2.4); low back pain was the most strongly associated with CP (PR=2.2; 95% CI [confidence interval]=2.1-2.3) and HICP (PR=2.3; 95% CI=2.1-2.5) (Table). Among adults with arthritis, 5 subgroups had CP prevalence >70%: serious psychological distress (82.2%), unable to work/disabled (80.8%), neck pain (74.1%), fair/poor self-rated health (73.3%), and arthritis-attributable activity limitations (71.7%). At least 40% in these 5 subgroups had HICP: unable to work/disabled (63.4%), serious psychological distress (59.7%), American Indian/Alaskan Native (43.0%), kidney disease (41.1%), and neck pain (40.3%).
Conclusion: Approximately one in two and one in five adults with arthritis live with CP and HICP, respectively; among them, both CP and HICP prevalence was even higher for those living with other challenges, including work disability and psychological distress. Despite unknown temporality, our study results combined with clinical evidence suggests that arthritis may be a leading cause of CP and HICP among US adults. Integrated approaches to pain management that include evidence-based non-pharmacologic strategies (e.g., cognitive behavioral therapy, physical activity, and self-management education) can reduce CP and its adverse effects, such as psychological distress, and may help reduce prescribed opioid use.
To cite this abstract in AMA style:
Murphy L, Theis K, Guglielmo D, Barbour K, Helmick C, Croft J. When It Just Won’t Stop: Chronic Pain and High Impact Chronic Pain Among U.S. Adults with Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/when-it-just-wont-stop-chronic-pain-and-high-impact-chronic-pain-among-u-s-adults-with-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/when-it-just-wont-stop-chronic-pain-and-high-impact-chronic-pain-among-u-s-adults-with-arthritis/