Session Information
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Psoriasis (Pso) is a common chronic inflammatory skin disease. About 30% of Pso patients develop psoriatic arthritis (PsA), a chronic inflammation of joints and entheses with an additional negative impact on quality of life. Early detection of PsA patients is important to ensure timely treatment and prevention of structural joint damage. Unfortunately, PsA is markedly under-diagnosed by dermatologists; an unmet need for biomarker-profiles to screen Pso patients at-risk is obvious. The aim of our study was to assess whether high dimensional flowcytometric profiling can distinguish Pso and PsA patients.
Methods: A cross-sectional and case-control study recruited 25 Pso patients without arthritis and 33 patients with PsA, both not using biological therapy at baseline. Psoriasis was diagnosed by a dermatologist and all the included Pso patients had a Psoriasis Epidemiology Screening Tool (PEST) score of 2 or lower. All PsA patients were clinically diagnosed by a rheumatologist.
Peripheral blood samples were analyzed by high dimensional flowcytometry, consisting of five different and supplementary 10-color antibody panels, which enables the characterization of ~150 immune cell populations. Both semi-unsupervised and unsupervised computational flow cytometry analyses were performed. In case of semi-unsupervised analysis, the flow cytometry data was first manually analysed, followed by principal component analysis (PCA) and unsupervised hierarchical clustering of PCA (HCPC). For unsupervised computational flow cytometry, flowsom and viSNE analysis packages of Cytobank were used.
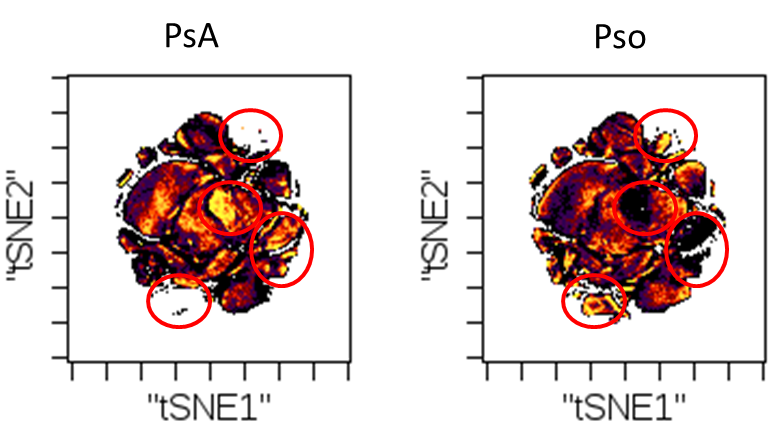
Results: The PsA and Pso population were comparable with regard to gender. In line with expectations, the PsA patients were slightly older compared to the Pso patients (57±15.4 vs 44±14.6). There was a significant difference in the use of methotrexate between the PsA patients (51%) and Pso patients (12%). Semi-unsupervised analysis of high dimensional flow cytometry data of peripheral blood from Pso and PsA patients clearly revealed differential clustering of Pso-vs-PsA patients as indicated by principal component analysis (Fig 1). This distinction between Pso and PsA patients was independent of age, gender, PASI scores and methotrexate use. Also unsupervised clustering showed a clear distinction between both diseases. Similar, unsupervised computational analysis utilizing flowsom and viSNE showed marked differences in the immune cell subset profiles between Pso and PsA patients (Fig 2).
Conclusion: High dimensional flowcytometric evaluation with semi-unsupervised and unsupervised analysis, can differentiate Pso and PsA patiens. Following validation, the obtained immune profiles might be used to support the timely diagnosis of PsA in Pso patients, as well as target finding to prevent this disease-shift.
To cite this abstract in AMA style:
Mulder M, van den Reek J, de Jong E, van Cranenbroek B, Smeets R, Joosten I, He X, van den Hoogen F, Koenen H, Wenink M. High Dimensional Flowcytometric Profiling Distinguishes Psoriasis and Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/high-dimensional-flowcytometric-profiling-distinguishes-psoriasis-and-psoriatic-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/high-dimensional-flowcytometric-profiling-distinguishes-psoriasis-and-psoriatic-arthritis/