Session Information
Date: Monday, November 11, 2019
Title: 4M118: Reproductive Issues in Rheumatic Disorders (1896–1901)
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: For many women, breastfeeding is a central aspect of motherhood, but many worry that their rheumatic disease or treatment will interfere. Fortunately, most anti-rheumatic medications are compatible with breastfeeding. This study sought to identify the frequency and predictors of the desire to and actually breastfeeding in women with a range of rheumatic diseases.
Methods: All pregnant patients with rheumatic disease in a single center between 2008-2018 in a prospective study of pregnancy and the post-partum period. Women were grouped into 4 diagnosis categories: systemic lupus erythematosus (SLE), undifferentiated connective tissue disease (UCTD), inflammatory arthritis (including rheumatoid, psoriatic, juvenile idiopathic arthritis, and spondyloarthropathies) and other rare rheumatic diseases. Breastfeeding intention was collected at study entry and breastfeeding was recorded at the post-partum visit. Infant feeding was divided into those who exclusively formula-fed, compared to those who exclusively breastfed or fed with a combination of breastmilk and formula.
Results: A total of 265 pregnancies were included in the study, 88 with SLE, 33 with UCTD, 100 with arthritis, and 44 with other rheumatic diagnoses. Overall, most patients were white (70%), had at least a college education (71%), lived with a spouse/partner (85%), and had private health insurance (76%). While pregnant, % of all women indicated a desire and plan to breastfeed their infant.
Post-partum, an average of 7.5 weeks after delivery, 92 (35%) were feeding exclusively with formula, 110 (42%) exclusively breastmilk, and 63 (24%) a mix of breastmilk and formula. Of the women who planned to formula-feed only, 85% did so. On the other hand, 25% of the women who planned to breastfeed were not. Of these, 81 had tried to breastfeed, but stopped. The most common reasons for having breastfeeding were having a low milk supply, the baby being unwell, and concerns over the mother’s medications.
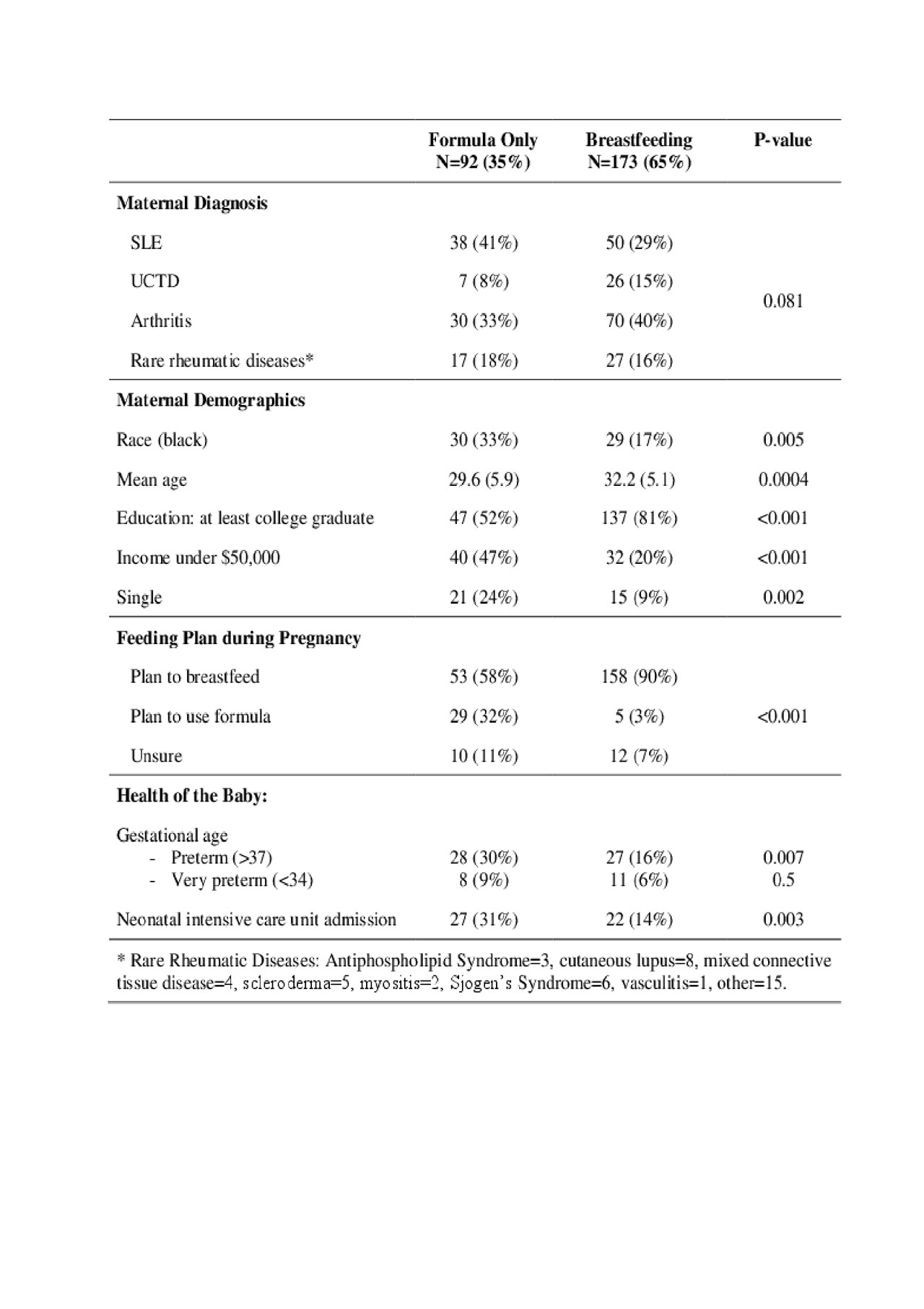
In univariate analysis, exclusively feeding with formula was not associated with maternal diagnosis, but was significantly more common in women who were black, younger, had less than a college education, had an income under $50,000/year, and live without a partner (see Table 1). Babies that were admitted to the neonatal intensive care unit or were born preterm were more likely to be formula-fed. In analysis, formula feeding was only associated with preterm delivery (OR 2.97 (1.39, 6.35)), younger maternal age (OR 0.94 (0.88-1.00)) and the mother having a college degree (OR 0.33 (0.17, 0.66)). Maternal education trumped race: only 30% of black women and 25% of non-black women with a college degree fed exclusively with formula.
Conclusion: The large majority of women with rheumatic disease in this cohort planned to breastfeed and were breastfeeding at follow-up. Maternal education and preterm birth were the primary predictors of breastfeeding, while diagnosis and race did not significantly impact the frequency of breastfeeding. The majority of women with rheumatic disease want to breastfeed and, given the safety of our medications for lactation, the large majority can do so successfully.
To cite this abstract in AMA style:
Ikram N, Eudy A, Clowse M. Breastfeeding in Women with Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/breastfeeding-in-women-with-rheumatic-diseases/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/breastfeeding-in-women-with-rheumatic-diseases/