Session Information
Session Type: ACR Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: The pathogenesis of neuropsychiatric Systemic Lupus Erythematosus (NPSLE) is incompletely understood, but is considered to be complex and multifactorial. Additionally, there is a wide range of possible NPSLE manifestations, including cognitive abnormalities, mood disorders, confusion, psychosis, and seizures. We have recently proposed that the blood-cerebrospinal fluid barrier at the brain choroid plexus (CP), rather than the blood-brain barrier, is the entry site for lymphocytes and other neuroinflammatory mediators into the brain. Indeed, the choroid plexus in the spontaneous MRL/lpr lupus mouse model is heavily infiltrated with predominantly T follicular helper CD4+ T cells and B cells, while preliminary imaging studies in human NPSLE have similarly revealed inflammation in the region of the CP. However, the function of CP-infiltrating T cells has not been studied as a potential contributor to the pathogenesis of NPSLE.
Methods: Six week old female MRL/lpr mice were intracerebroventricularly (ICV) injected with either MRL/lpr choroid plexus CD3+ T cells (n=6), MRL/lpr splenic CD3+ T cells (n=5), or PBS (n=4). The T cells were pooled from the choroid plexus of 16 week old MRL/lpr mice (n=7) and from the spleen of 6 week old MRL/lpr mice (n=2). The cells were stimulated and expanded with anti-CD3/CD28 antibodies (1 ug/mL) and mIL-2 (10 U/mL) for 4 days. About ~200,000 cells were injected into the lateral ventricle from the bregma at AP -0.34 mm, ML -1.0 mm, and depth -2.0 mm. Mice were sacrificed 4 weeks post-injection, with behavioral assessments and histology performed to assess features of NPSLE.
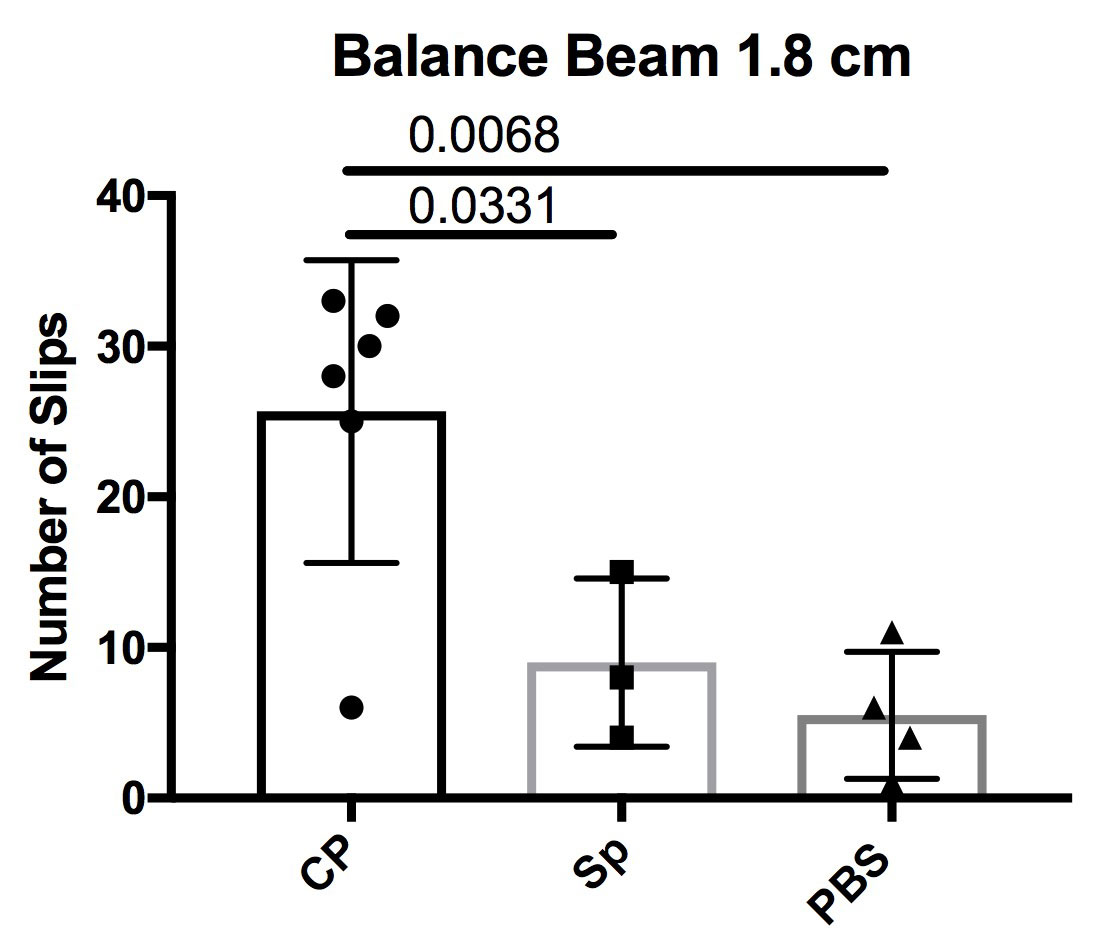
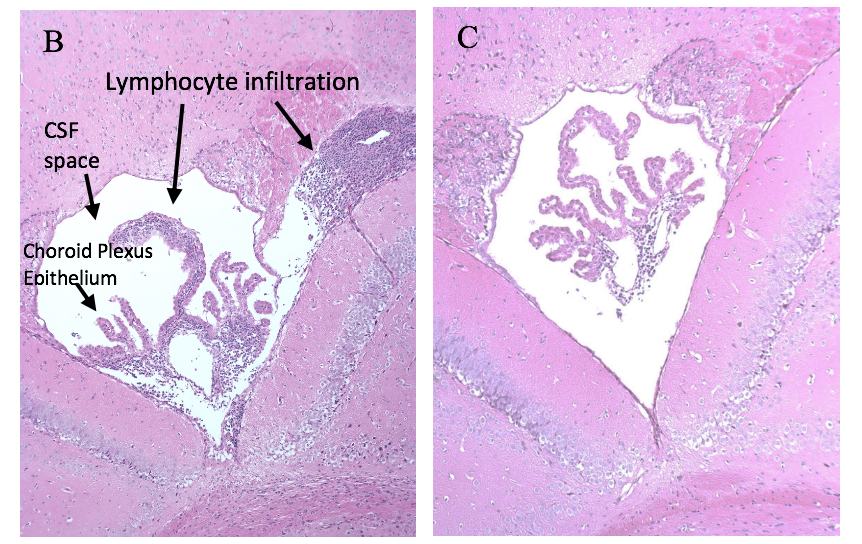
Results: In this pilot study, we found that CP T cell recipient mice had increased cognitive and depressive deficits compared to PBS controls and the MRL/lpr splenic T cell recipient mice. Additionally, the CP T cell recipient mice had a significantly compromised motor function, as assessed by the number of slips while crossing a balance beam (p = 0.0068), when compared to the splenocyte injected groups and the PBS controls (Figure 1A). Histological assessment and immunohistochemical staining revealed an increase in lymphocytic infiltration, the number of proliferating cells (Figure 1B-C), as well as in IgG and complement deposition, in the choroid plexus of CP T recipient mice compared to the PBS group.
Conclusion: Our result indicate that T cells can migrate to and proliferate in the CP following ICV injection, and that brain infiltrating MRL/lpr T cells may be a key contributor to the pathogenesis of NPSLE.
To cite this abstract in AMA style:
Moore E, Huang M, Reynolds C, Putterman C. The Pathogenic Potential of Choroid Plexus T Cells in Neuropsychiatric Lupus [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-pathogenic-potential-of-choroid-plexus-t-cells-in-neuropsychiatric-lupus/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-pathogenic-potential-of-choroid-plexus-t-cells-in-neuropsychiatric-lupus/