Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: ANCA-associated vasculitis (AAV) is a small vessel vasculitis associated with an intense inflammatory state. AAV patients are at a 2-fold higher risk of cardiovascular disease (CVD) compared to the general population and CVD is the leading cause of death in this population. As such, CVD risk stratification, often with lipid levels, is recommended in AAV. However, the effect of inflammation on lipid levels in AAV is poorly understood and may impact the interpretation of risk stratification. We sought to evaluate the association between AAV and lipid levels.
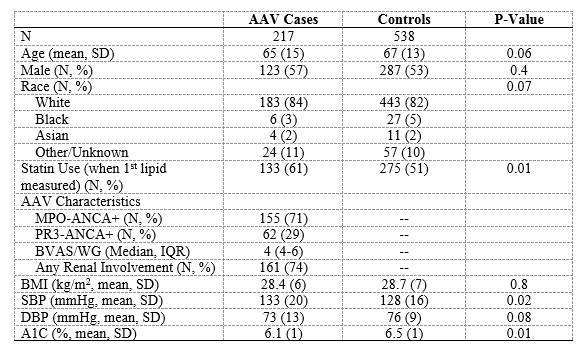
Methods: The Partners AAV (PAAV) cohort is a consecutive inception cohort established in the Partners HealthCare System (PHS), a large hospital system in New England. The PAAV cohort has been previously described. All cases are PR3- or MPO-ANCA+. Each AAV case was matched to up to five controls from the PHS Research Patient Data Registry by age, sex, race, and index date (date of AAV treatment initiation). We identified matched cases and controls who had lipid levels (total cholesterol [TC], high-density lipoprotein cholesterol [HDL-C], and low-density lipoprotein cholesterol [LDL-C]) measured as part of routine care following the index date. The primary outcome of interest was the difference in lipid levels between cases and controls using the first available lipid level within one year of the index date. We also evaluated the difference in lipid levels between AAV cases and controls in the second and third years of follow-up after the index date. We compared lipid levels between cases and controls using linear regression after adjusting for relevant covariates.
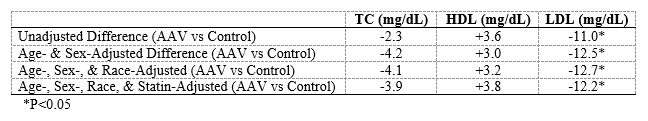
Results: We included 217 cases and 538 matched controls with lipid levels measured in the first year following the index date. The mean age (65 vs 67) and proportion of males (57% vs 53%) and White persons (84% vs 82%) was similar in cases and controls. The majority of AAV cases were MPO-ANCA+ (155, 71%). Compared with controls, AAV cases were more frequently prescribed a statin prior to the lipid measurement (61% vs 51%). In unadjusted analyses, TC (187 mg/dL vs 189 mg/dL, P= 0.62) and HDL-C (57 mg/dL vs 52 mg/dL, P= 0.08) were similar between cases and controls. In contrast, LDL-C was significantly lower in cases compared with controls (98 mg/dL vs 109 mg/dL, P=0.006). In analyses adjusted for age, sex, race, and statin use, AAV cases had a significantly lower LDL-C compared with controls (β= – 12.2 mg/dL (95% CI: -20.0 to -4.4), P= 0.002). During follow-up, the difference in LDL-C between cases and controls were no longer significant (Year 2: β= -8.9 mg/dL (95% CI: -19.0 to +1.3 ), P=0.09; Year 3: β= -5.2 mg/dL (95% CI: -16.4 to +6.1), P=0.4).
Conclusion: We found that LDL-C levels are significantly lower in AAV cases compared to controls in the first year following treatment initiation and these differences appear to dissipate subsequently. We hypothesize that this reflects improvements in the inflammatory state among AAV cases. When screening for dyslipidemia in AAV and assessing CVD risk, one should consider the effect of inflammation on lipid levels. Future studies are necessary to understand if lipid levels, especially as part of risk stratification tools, accurately predict CVD events in this population.
To cite this abstract in AMA style:
Wallace Z, Fu X, Zhang Y, Stone J, Choi H. The Association of Reduced Low-Density Lipoprotein (LDL) Cholesterol Levels with ANCA-Associated Vasculitis (AAV) [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-association-of-reduced-low-density-lipoprotein-ldl-cholesterol-levels-with-anca-associated-vasculitis-aav/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-association-of-reduced-low-density-lipoprotein-ldl-cholesterol-levels-with-anca-associated-vasculitis-aav/