Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: ANCA associated vasculitis patients have a wide spectrum of pulmonary involvement in the form nodular disease (especially peri-bronchial nodules), cavitating lesions, diffuse alveolar hemorrhage and less commonly interstitial lung disease (ILD) either usual interstitial pneumonitis (UIP) or nonspecific interstitial pneumonia (NSIP). ILD seems to be a rare manifestation mostly associated with MPA (Microscopic Polyangiitis). However, the disease characteristics, serologic findings, demographics and associated risk factors is not well described to date in this subset of patients.
Methods:
We performed a single center analysis of patients diagnosed with ANCA associated vasculitis (diagnosed based on biopsy findings and/or appropriate lab criteria with typical clinical characteristics) followed in the vasculitis clinic at Loma Linda University Health from 2017 to current. A retrospective chart analysis was performed on patients with diagnosis of AAV and ILD. Epidemiologic, demographic, clinical, imaging and serological data for these patients were collected. ILD was diagnosed by typical findings on CT scan, lung biopsy or restrictive pattern on PFTs in the absence of other potential causes of restrictive lung disease.
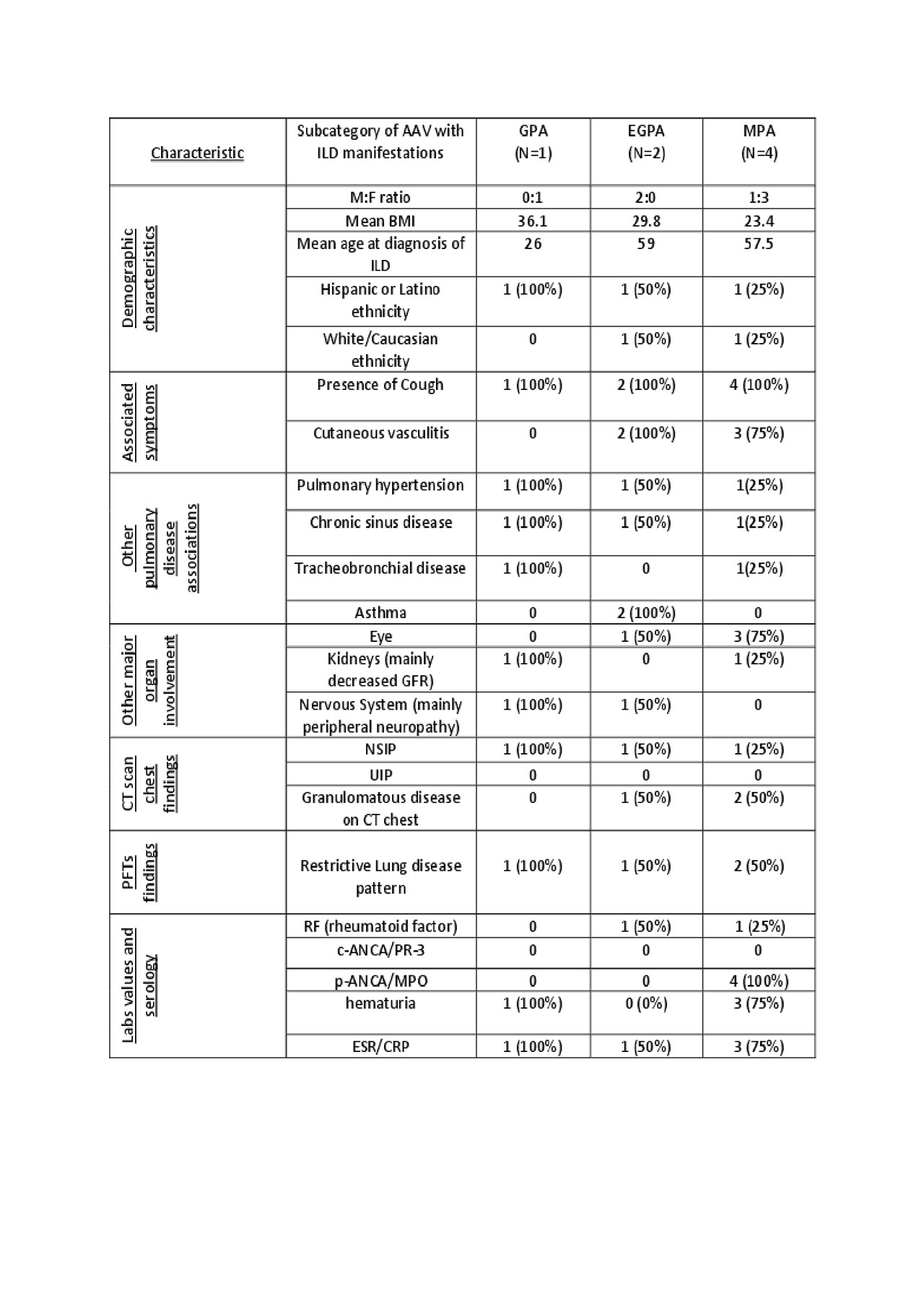
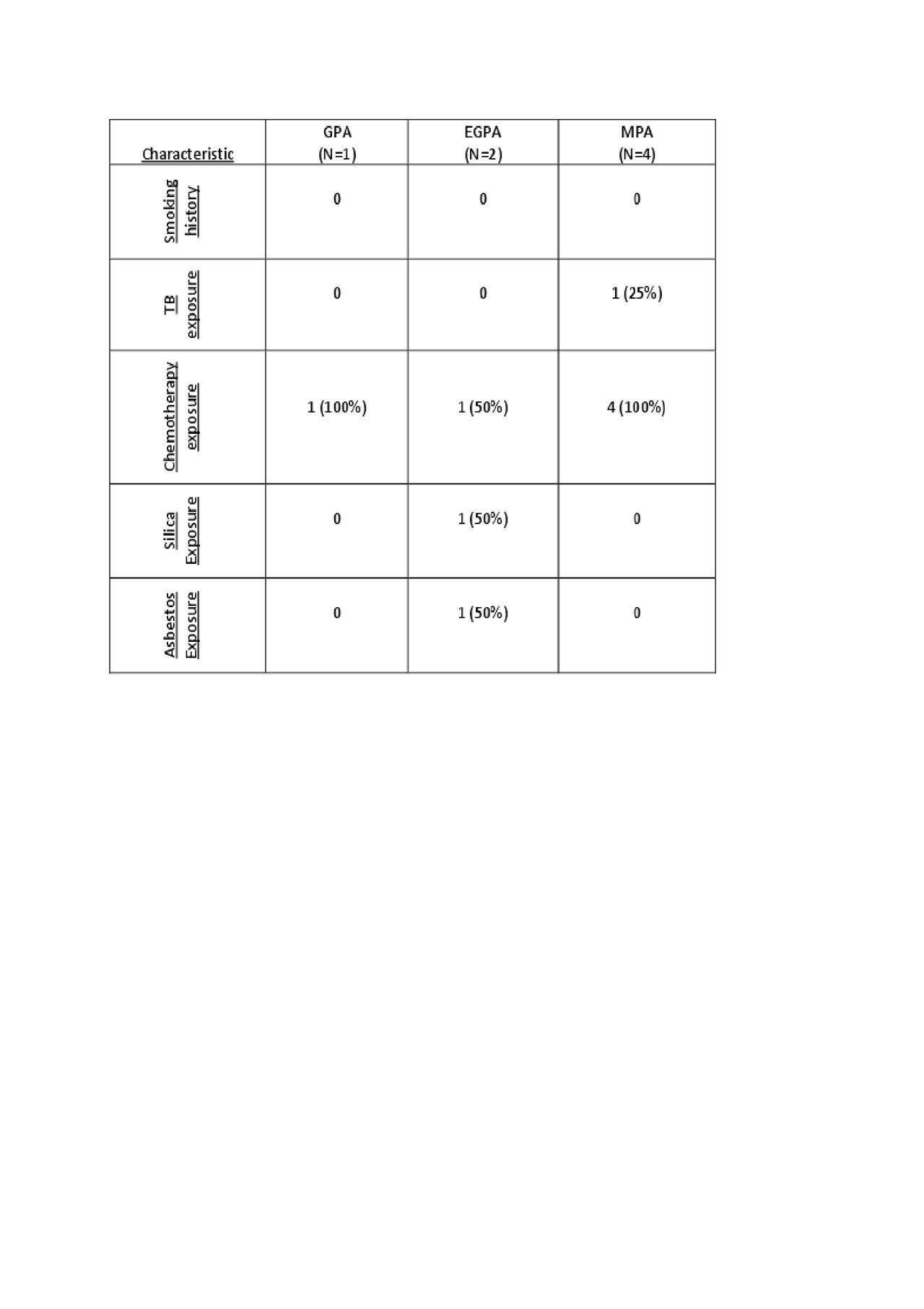
Results: Thirty patients with AAV (M:F= 8:22, mean age at diagnosis 51.3) were enrolled. 15 patients (50%) had Granulomatosis with Polyangiitis (GPA), 11 patients (36.6%) had Microscopic Polyangiitis (MPA) and 4 patients (13.3%) had Eosinophilic Granulomatosis with Polyangiitis (EGPA). ILD was diagnosed in 1 out of 15 GPA patients (6.6%), 2 out of 4 EGPA patients (50%) and 4 out of 11 MPA patients (36.3%). Mean time of diagnosis of ILD from the time of AAV diagnosis was 7 years in GPA, 9 months in EGPA and 10 years in MPA. 42.8% were of Hispanic/Latino ethnicity and 28.5% patients were of White/Caucasian ethnicity. Mean age of ILD diagnosis for GPA was noted to be 26 years as compared to EGPA and MPA which was 58.2 years. NSIP was the most frequent CT pattern found in all AAV patients with ILD in our cohort. None of the patients had any smoking history. TB exposure was reported in 1 patient and occupational asbestos and silica exposures were reported in 1 patient. All 7 patients had some degree of chronic prednisone use. 6 out of 7 patients received treatment with Rituximab and 1 patient was treated with Cytoxan for their AAV. Of note the 2 patients that had associated kidney disease were found to have pauci-immune crescentic GN on kidney biopsy.
Conclusion:
Our study revealed ILD is most seen in MPA and least common in GPA. It is strongly associated with MPO Abs. ILD tends to present earlier through the course of the disease in EGPA patients as compared to MPA and GPA patients. Chronic sinusitis and pulmonary hypertension were the most frequent concurrent pulmonary manifestations while cutaneous vasculitis and eye involvement seems to be the most common extra-pulmonary manifestations. None of the patients with AAV-ILD had a smoking history. Although hematuria was a common manifestation observed in most AAV-ILD patients, decreased GFR was only observed in 2 patients. Further prospective studies in larger cohorts are required to clarify the clinical characteristics and prognosis of ILD in patients with AAV.
To cite this abstract in AMA style:
Youssef H, Hojjati M. Interstitial Lung Disease in ANCA Associated Vasculitis: A Single Center Retrospective Analysis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/interstitial-lung-disease-in-anca-associated-vasculitis-a-single-center-retrospective-analysis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/interstitial-lung-disease-in-anca-associated-vasculitis-a-single-center-retrospective-analysis/