Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Lupus is a systemic autoimmune disease whose mechanism of development is largely unknown. Prior infection is a suspected sentinel event that may trigger disease in susceptible people and have an impact on disease development. In this exploratory study, we investigated if severe infections prior to SLE diagnosis were associated with specific SLE attributes and comorbidities.
Methods: We identified 469 patients with known SLE in a physician validated registry, the Chicago Lupus Database, with medical records in the Northwestern Medicine Enterprise Data Warehouse (NMEDW). Each patient was assessed for the Systemic Lupus International Collaborating Clinics classification (SLICC) criteria, via chart review, to determine the presence or absence of each criteria. We excluded ANA from the analysis because 15% patients had missing ANA values (likely due to tests being performed at an outside institutions). Prior severe infections (viral, bacterial, fungal and mycobacterial) and comorbidities (heart failure, stroke, sepsis, end stage renal disease and osteoporosis) were identified based on ICD9/10 codes in the NMEDW. The association between prior infections and SLE criteria and comorbidities were evaluated using multivariate logistic regression. Models were adjusted for age of SLE onset, sex and race/ethnicity. Severe viral and bacterial infections were also analyzed separately in relation to criteria and comorbidities to assess associations.
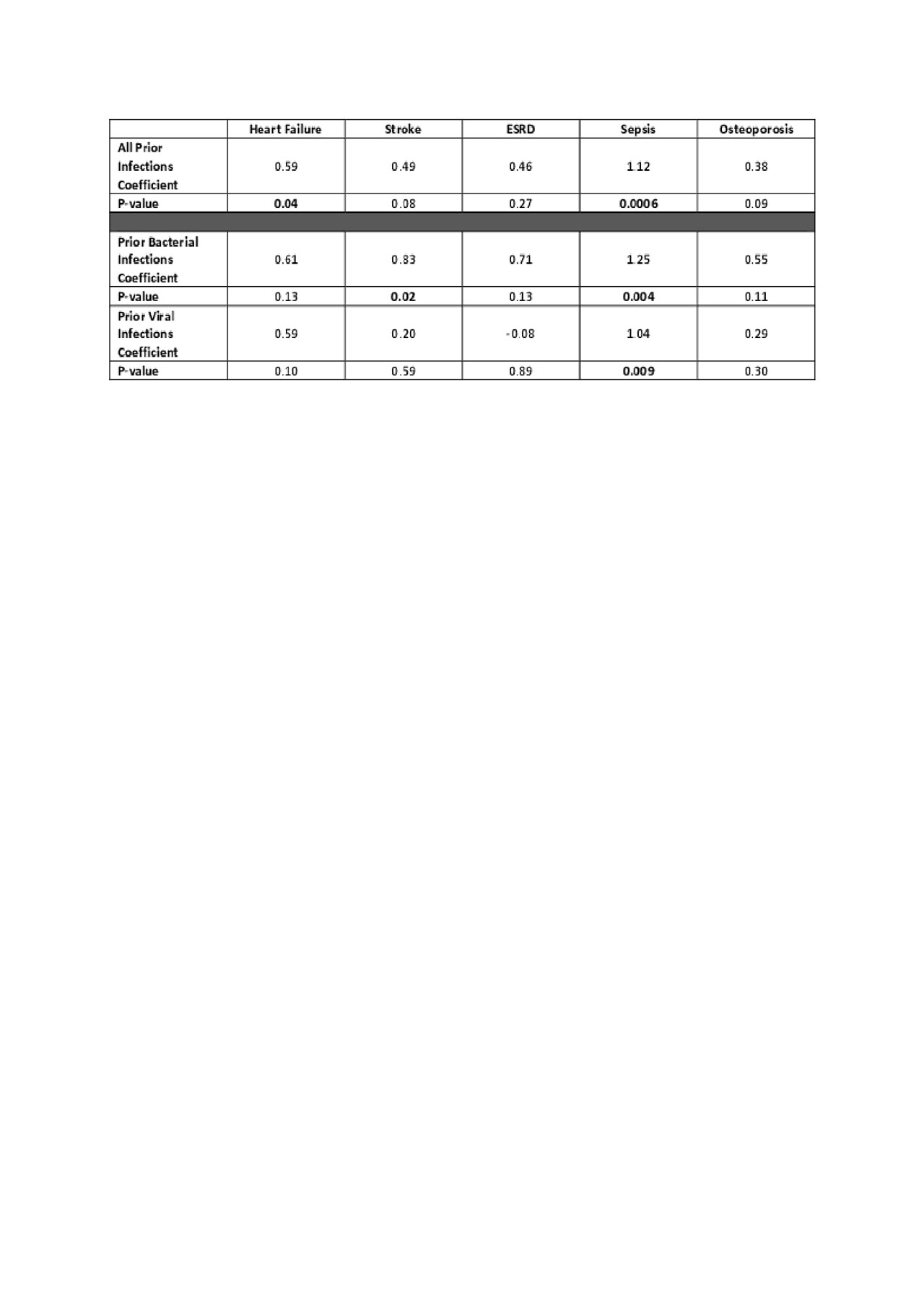
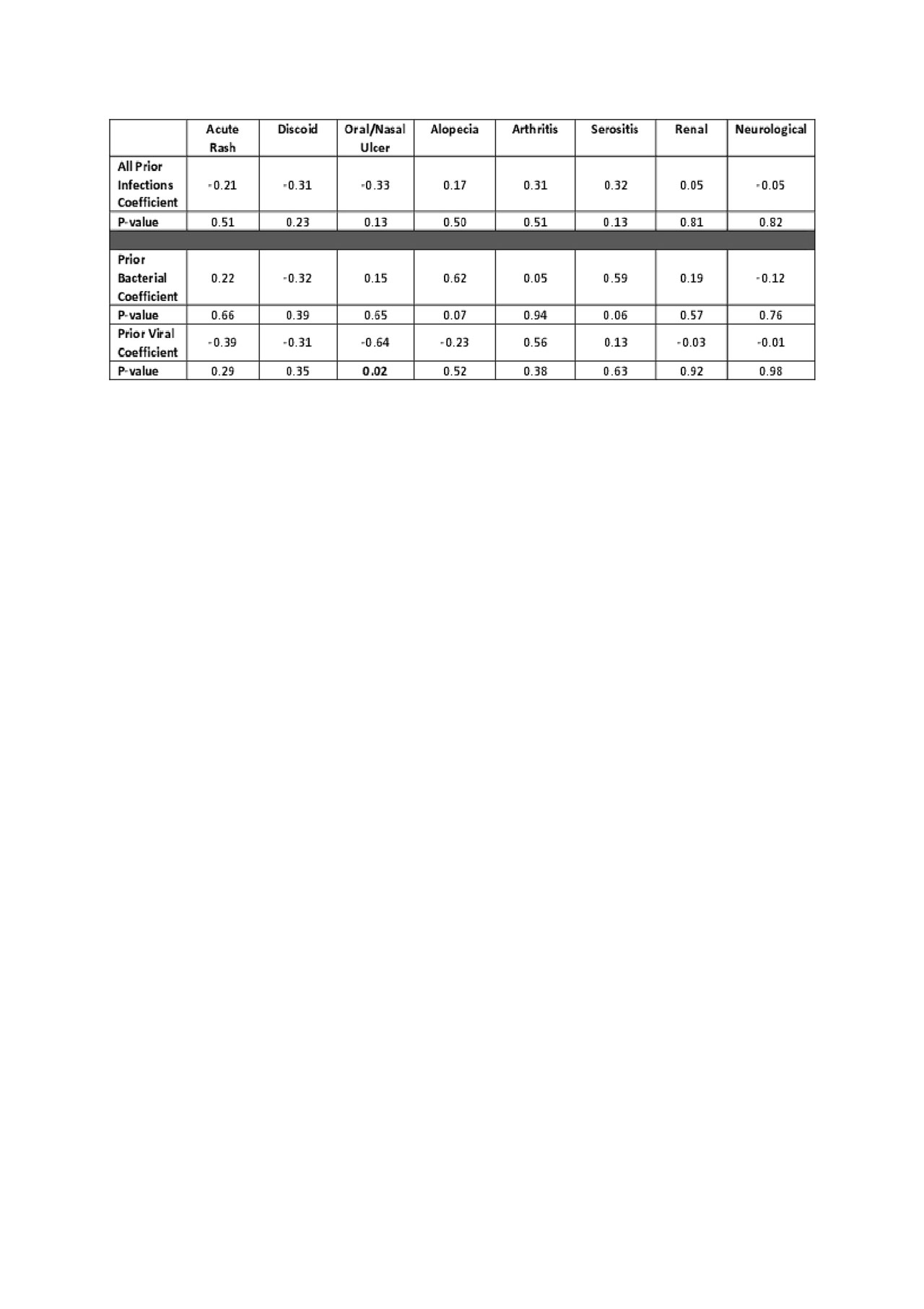
Results: Among 469 patients, 26% had severe infections prior to SLE diagnosis, including 71 with viral infections and 49 with bacterial infections. The average age of SLE diagnosis in our population is 30.1 years; 50% are white, 29% African American, 21% identified in other racial/ethnic categories; 92% are female. For SLE comorbidities, 14% developed heart failure, 15% had a stroke, 9% developed ESRD, and 58% developed osteoporosis. Association coefficients and p-values between infection prior to diagnosis of SLE and classification criteria are shown in Tables 1a and 1b and the relation between infections and comorbidities are shown in Table 2. Among classification criteria, prior infection is significantly associated with leukopenia (p=0.03). Among comorbidities, prior infection is significantly associated with heart failure and sepsis. When analyzing prior infections by viral and bacterial subgroups, bacterial infections had significant association with stroke (p=0.02) and sepsis (p= 0.004). Viral infections were significantly associated with oral ulcers (p=0.02) and sepsis (p= 0.009). Association between prior bacterial infection and alopecia (p= 0.07), serositis (0.06), as well as association between prior viral infection and leukopenia (p = 0.08) had borderline significance.
Conclusion: Our exploratory study shows severe infections prior to SLE diagnosis are associated with leukopenia, oral ulcers and an increased risk of heart failure, stroke and sepsis. These results suggest that prior infection could increase the likelihood of long term cardiovascular comorbidities, and that supportive care should be considered to minimize infections and cardiovascular complications for persons with SLE.
ACR2109.Table1a.Final.20190604

ACR2109.Table1b.Final.20190604
To cite this abstract in AMA style:
Deng Y, Chung A, Kho A, Luo Y, Ramsey-Goldman R, Walunas T. Severe Infection Prior to Diagnosis of Systemic Lupus Erythematosus (SLE) Is Associated with Disease-Specific Attributes and Long-Term Comorbidities [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/severe-infection-prior-to-diagnosis-of-systemic-lupus-erythematosus-sle-is-associated-with-disease-specific-attributes-and-long-term-comorbidities/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/severe-infection-prior-to-diagnosis-of-systemic-lupus-erythematosus-sle-is-associated-with-disease-specific-attributes-and-long-term-comorbidities/