Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic Lupus Erithematosus (SLE) is associated with increased cardiovascular (CV) risk compared with general population; an accelerated atherosclerosis is considered the main underlying mechanism. Arterial Stiffness (AS) is considered a reliable surrogate marker of arterial wall dysfunction and an independent predictor of cardiovascular events in the general population. Several studies showed that AS in SLE patients is abnormally increased with respect to healthy controls; however, the prognostic value of AS has not been fully evaluated in patients with SLE. The aim of the study was to evaluate the predictive value of AS for major cardiovascular events, mortality and poor renal outcome in SLE patients.
Methods: Consecutive SLE patients classified according to the 1997 ACR criteria were enrolled for this study. At baseline, demographics, clinical history, menopause status, cumulative dose of glucocorticoid (GC), traditional CV risk factors, disease activity and organ damage (according to SELENA-SLEDAI and SLICC/DI respectively) were recorded; AS was assessed by measuring carotid-femoral pulse wave velocity (PWV). The patients were prospectively followed, and the following outcomes were evaluated at last observation: major events (including IMA, PTCA, mortality due to CV events, overall mortality, stroke, TIA); poor renal outcome (end-stage renal disease, dialysis or renal transplantation).
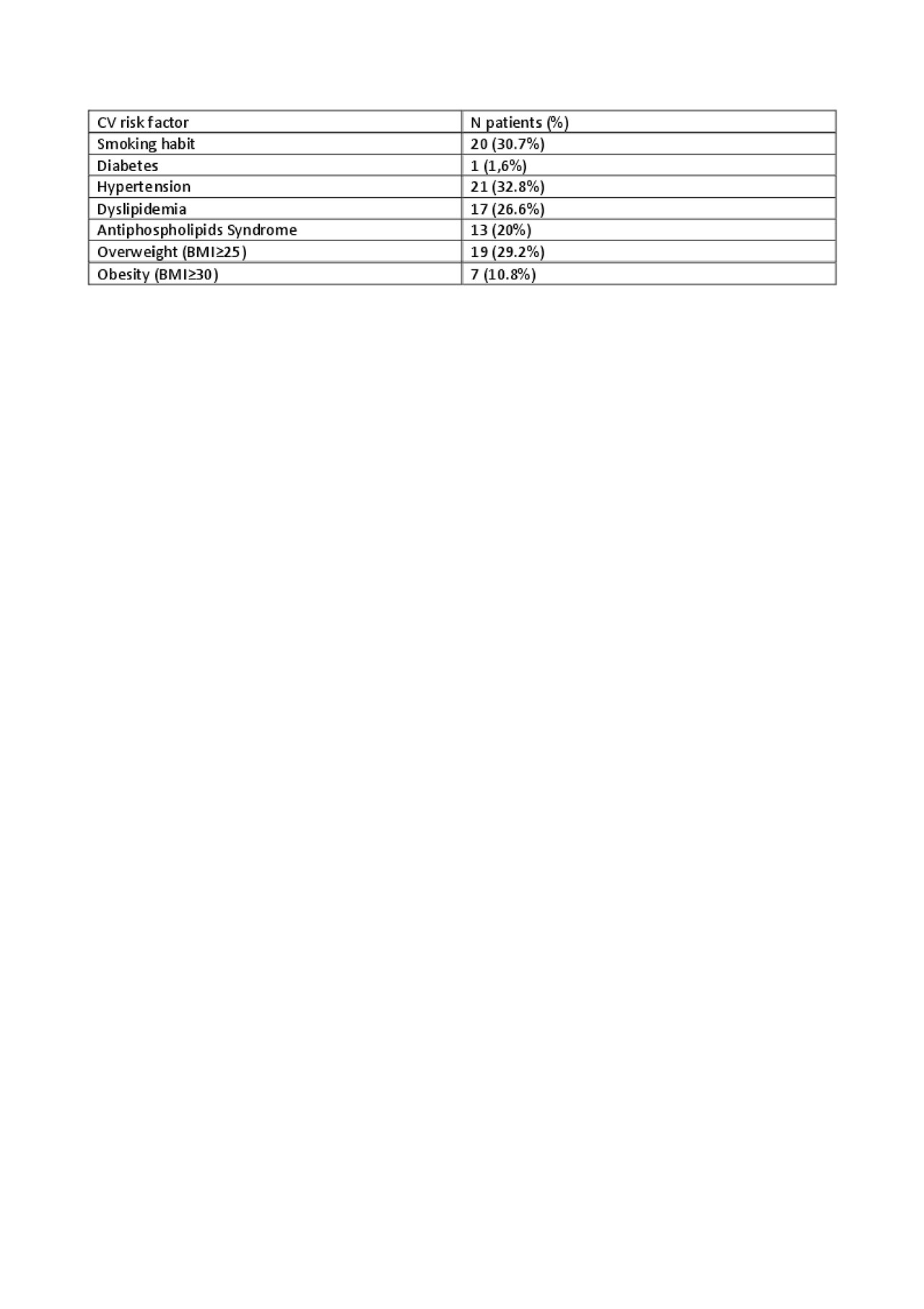
Results: A total of 65 patients were included (63 Caucasian, %, 63 females, %). At baseline, median age was 41.5 ± 11.9 years, median disease duration was 14 years (IQR 9-24). As for cumulative organ involvement, the most prevalent was cutaneous involvement (n= 48, 75%), followed by renal (n=31, 48.4%), serositis (n=10, 15.6%) and neuropsychiatric (n=10, 15.6%). Cumulative median dose of GC was 16.75 g (IQR 10.25-30.00). Fifteen patients (23.1%) presented active disease (SLEDAI >4) at the time of enrolment, 19 (29.2%) had at least one organ damage (SLICC >0); in those patients the median SLICC-DI resulted 2 (IQR 1-3). The prevalence of traditional CV risk factors is reported in table 1. Overall, at baseline PWV resulted 7 (IQR 6.35-8.45) and vascular age 48 (IQR 39.3-60.0). During the observational period (mean duration of follow-up 4.5 ± 2.4 years), 7 major events occurred in seven patients (10.8%), namely: 5 patients suffered from IMA, 1 from stroke; one death also occurred, for non-CV cause (sepsis). Only one patient developed a poor renal outcome, requiring dialytic treatment and then renal transplant. CV events occurred at median age of 43.8±9.8 years. At univariate cox-regression analysis, baseline age (OR= 1.078 ) , PWV (OR= 1.71) and vascular age (OR= 1.08) all resulted predictors of future major events (p< 0.01; p< 0.01; p< 0.02 respectively); baseline SLICC was also predictive of major events (p< 0.01).
Conclusion: These data suggest that arterial stiffness could be considered a reliable marker of early vascular aging in patients with SLE and its predictive value for cardiovascular events was confirmed in this population. Thus, these data support the utility of the vascular ageing assessment to set-up preventive strategies tailored on the single patient.
To cite this abstract in AMA style:
Signorini V, Zucchi D, Tani C, Bruno R, Elefante E, Stagnaro C, Carli L, Parma A, Ferro F, Armenia S, Ghiadoni l, Taddei S, Mosca M. Early Vascular Ageing as a Predictor of Future Cardiovascular Events and Mortality in Systemic Lupus Erythematosus Patients: A Prospective Cohort Study [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/early-vascular-ageing-as-a-predictor-of-future-cardiovascular-events-and-mortality-in-systemic-lupus-erythematosus-patients-a-prospective-cohort-study/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/early-vascular-ageing-as-a-predictor-of-future-cardiovascular-events-and-mortality-in-systemic-lupus-erythematosus-patients-a-prospective-cohort-study/