Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: The prevalence of peripheral neurological manifestations in Systemic Lupus Erythematosus (SLE) ranges between 1.5% and 27% and are a major cause of morbidity.
To determine associated factors with the different neurophysiological patterns in peripheral neuropathies in patients with systemic lupus erythematosus.
Methods: A retrospective study was performed. We included patients with SLE (ACR 1997 and SLICC 2012 criteria), who presented a PNP associated with SLE according to ACR 1999 nomenclature, from January 2014 to December 2018. Patients were classified according to the neurophysiologic pattern by the Neuromuscular Clinic Disorders at our Institute in 3 groups: 1. Sensory or sensory-motor axonal neuropathy (ANP). 2. Multiplex Mononeuropathy (MNP), and 3. Demyelinating neuropathy (DNP). Clinical information including demographics and SLE characteristics were gathered from the clinical chart and reviewed by an expert rheumatologist in three different moments: Previous visit (3 months before to PNP presentation); at the time of PNP presentation, and one year after. Demographic characteristics: gender, age, Body Mass Index (BMI), and comorbidities. Lupus characteristics: ACR criteria, the time between SLE diagnosis and PNP presentation, ACR / 2012 criteria, disease activity (SLEDAI-2K), cumulative damage (ACR/SLICC-DI), and treatment were compared. One year after, disease activity, cumulative damage, and treatment were reviewed. Statistical analysis: Mann-Whitney U, Chi-squared test and Fisher exact test were used as appropriate. Multiple comparisons and logistic regression analysis was made.
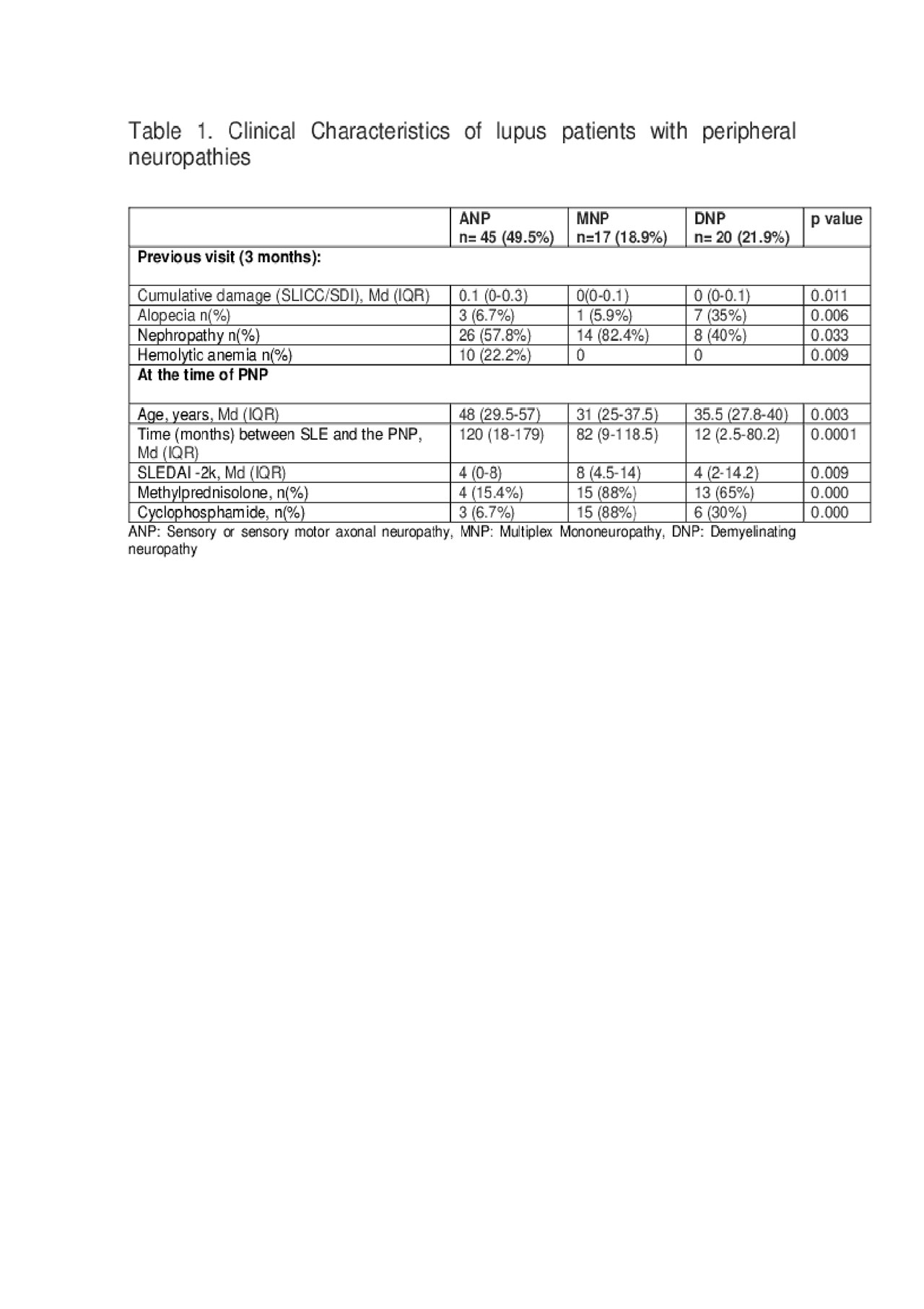
Results: Ninety one PNP were included, 45 (49.5%) ANP, 17 (18.9%) MNP, and 20 (21.9%) DNP. Demographics and comorbidities were similar between groups. At previous visit, the (SLICC/SDI) was higher in APN group compared with MNP and DNP (table 1). Patients with DNP presented more frequently cutaneous manifestations (alopecia) compared with MNP and ANP (table1). Patients with MNP had more nephropathy compared with ANP and DNP, and patients with APN had more hemolytic anemia compared with other groups (table 1).
At the time of PNP presentation, patients with ANP were older and had a long time between SLE diagnosis and the PNP presentation, compared with MNP and with DNP (table 1). Patients with MNP had higher disease activity compared with ANP and DNP groups (table 1). Pulses of methylprednisolone, cyclophosphamide, and higher doses of prednisone were used in the MNP compared with DNP and ANP group (p < 0.05). One year after, disease activity and cumulative damage were similar between groups. In the logistic regression analyses, older age, the time between SLE diagnosis and PNP presentation, and cumulative damage in the previous visit were factors independently associated with APN compared with MNP and DNP (table 2).
Conclusion: ANP was the most frequent PNP. Patients with MNP have more disease activity than the other groups. MNP and DNP considered more severe and received more aggressive treatment than APN. Factors independently associated with APN were older age, have a longer time between SLE diagnosis and the PNP presentation and have more damage 3 months previous the PNP presentation.
To cite this abstract in AMA style:
Garcia-Guevara G, Treviño-Tello F, Cabib C, Contreras-Yáñez I, Chiquete E, Díaz-Mora A, Fernandez-Nicoli Y, Macias-Gallardo J, Gómez-Piña J, Sandoval-Flores I, Fragoso-Loyo H. Factors Associated with Peripheral Neuropathies in Patients with Systemic Lupus Erythematosus: A Single Center Experience [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/factors-associated-with-peripheral-neuropathies-in-patients-with-systemic-lupus-erythematosus-a-single-center-experience/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-associated-with-peripheral-neuropathies-in-patients-with-systemic-lupus-erythematosus-a-single-center-experience/