Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Homocysteinemia is present 8-15% of patients with SLE and is associated with increased risk of atherosclerosis, arterial thrombosis and stroke in SLE patients. Recently, it was found to be an independent predictor of new damage accrual in Mestizo SLE patients. The aim of this study was to determine the association between homocysteinemia and episodes of renal insufficiency.
Methods: A total of 1,688 SLE patients, diagnosed according to the SLICC or ACR classification criteria, had at least one homocysteine measurement. Among these, 341 had two visits with homocysteine measurement, 572 had three or more. Patients were followed quarterly per protocol. First, patients were classified as having homocysteinemia if their average homocysteine level was above 15 umol/L. and demographic and clinical subgroups were compared with respect to prevalence of homocysteinemia. Second, we used a longitudinal regression model to explore whether homocysteine levels were associated with serum creatinine levels longitudinally. Third, to assess whether a history of homocysteine was associated with episodes of renal insufficiency, we assessed whether there was a relationship between past measures of homocysteine and episodes of renal insufficiency (defined as serum creatinine exceeding 1.5 mg/dl). For each visit, we calculated the mean homocysteine level based on previous homocysteine levels and those with a mean level over 15 mg/dl were considered as a visit with previous homocysteinemia. We used a multivariable GEE model to assess the association between previous homocysteinemia and later renal insufficiency.
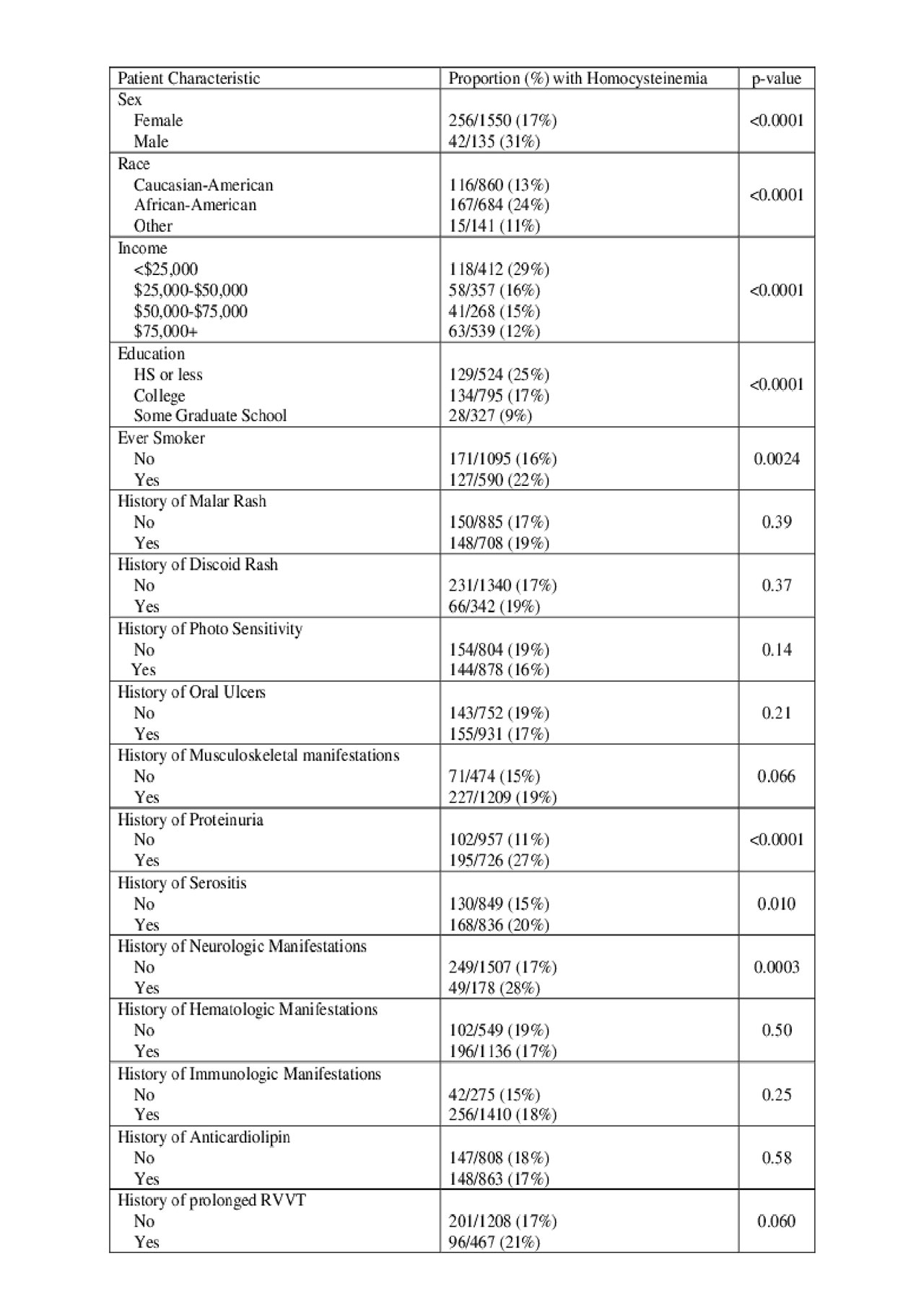
Results: 295 of the patients (17.7%) had homocysteinemia. Patients who were male, African-American, had a smoking history, proteinuria, and neurological manifestations were more likely to have homocysteinemia (Table 1). In the longitudinal analysis, we observed that those patients with generally higher levels of homocysteine tended to have higher levels of serum creatinine and that changes in homocysteine coincided with changes in serum creatinine. Specifically, a 1 umol /L increase in mean homocysteine levels was associated with a 0.04 mg/dl increase in serum creatinine (CI: 0.03, 0.04) (p< 0.0001). To assess the relationship between homocysteine and episodes of renal insufficiency, 10779 visits were identified after homocysteinemia, while 43651visits occurred following normal homocysteine levels. The proportion of visits with renal insufficiency was significantly higher in visits following a history of homocysteinemia (21% vs 3%). This association remained significant after adjusting for age, gender, ethnicity, hydroxychloroquine use, previous low C3, and previous proteinuria (CI: 2.7, 6.3) (p< .0001).
Conclusion: Homocysteinemia is a strong predictor of renal insufficiency even after adjusting for potential confounders. Homocysteine is a modifiable risk factor, as combination B-vitamins (B6, B12, and folic acid) can reduce it. Although treatment of homocysteinemia fell out of favor for prevention of cardiovascular outcomes, it should be reconsidered for the prevention of renal insufficiency. Longitudinal studies are needed.
To cite this abstract in AMA style:
Babaoglu H, Li J, Goldman D, Magder L, Petri M. Homocysteinemia Predicts Renal Insufficiency in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/homocysteinemia-predicts-renal-insufficiency-in-systemic-lupus-erythematosus/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/homocysteinemia-predicts-renal-insufficiency-in-systemic-lupus-erythematosus/