Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Evidence of podocyte effacement on electron microscopy and significant proteinuria in a systemic lupus erythematosus (SLE) patient with biopsy proven minimal mesangial (MM), mesangial proliferation (MsP) and focal segmental glomerulosclerosis (FSGS) is the defining quality of lupus podocytopathy (LP). Our objective is to recognize the prevalence of LP and significant proteinuria in SLE patients with biopsy proven class I, class II and/or FSGS.
Methods: In this single center retrospective study, two independent reviewers evaluated records from 96 hospitalized patients admitted with ICD-10 codes corresponding to a diagnosis of glomerular disease and/or tubulo-interstitial nephropathy in SLE from 2015 to 2018.
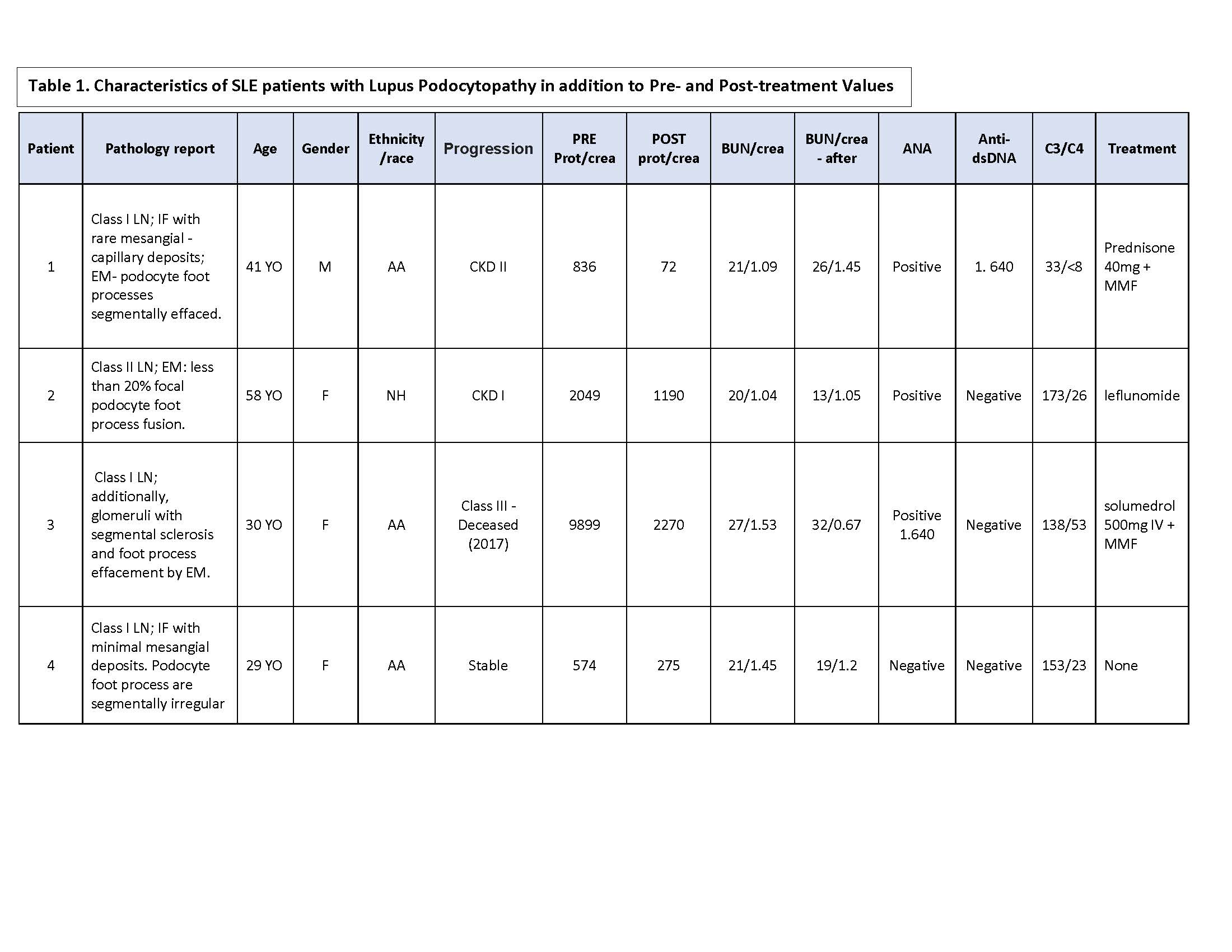
Results: The prevalence of LP in our cohort was 8.33% (Table 1). Seventy-five percent of our cohort were females and of African descent. Class II lupus nephritis (LN) was the most common pathological diagnosis (50% of patients); followed by class I LN (37.5%), and one case of FSGS (12.5%). Five patients presented with significant proteinuria (62.5%). Majority of the patients had active disease, presenting with low C3 levels (62.5%). Most patients received corticosteroids (CS), either pulse dose steroids or high dose prednisone being the most common mode (62.5%); four patients received a combination of CS and Mycophenolate mofetil (MMF). All of the patients treated with CS and MMF demonstrated greater than 50% improvement in the urine protein/creatinine ratio with mean duration of 27.5 days and persisted in remission. The patient with the FSGS pattern despite having greater than 50% improvement in protein/creatinine ratio relapsed to LN class III within 2 years.
Conclusion: It is important to recognize a subset of patients presenting with clinical signs of nephrotic syndrome despite biopsy demonstrating class I or class II LN. The literature outlines LP as a spectrum, from MM to FSGS, with worse response to treatment in patients with FSGS. [1] As demonstrated in our cohort of predominantly ethnic minorities with Class I and class II LN with LP patterns, majority had a favorable response to CS in combination with MMF; the only patient with the FSGS pattern underwent relapse. A larger cohort with longer duration of study period is needed to suggest recommendations for LP. It may be beneficial to treat LP in Class I and II LN when associated with proteinuria.
To cite this abstract in AMA style:
Bembry W, Lopez D, Mesa C, Patel N, Guevara M. Should Lupus Podocytopathy Be a Subclass in Class I and Class II Lupus Nephritis? [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/should-lupus-podocytopathy-be-a-subclass-in-class-i-and-class-ii-lupus-nephritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/should-lupus-podocytopathy-be-a-subclass-in-class-i-and-class-ii-lupus-nephritis/