Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: U-Act-Early was a 2-year multicentre, double-blind, randomized, placebo-controlled trial in early (DMARD-naïve) RA patients treated to the target of remission. Patients were assigned to step-up treatment strategies starting with tocilizumab (TCZ), methotrexate (MTX) or their combination (TCZ+MTX).1 If the treatment target was not achieved, MTX and/or TCZ was added. When patients achieved and remained in remission for ≥ 24 weeks, medication was tapered and finally stopped.1 Patients were followed for 3 years after the trial, during which treatment was at the discretion of the rheumatologist. The current study compares quality-adjusted life years (QALYs) and direct and indirect costs over 5 years between TCZ, MTX or TCZ+MTX initial strategy.
Methods: Costs were based on reported resource use and reference prices.2 QALYs were calculated based on the EQ5D using Dutch tariff.2 The economic evaluation considered all 317 randomized patients according to their allocated strategy group, using imputation with chained equations nested in bootstraps (5000 samples) to account for missing data and uncertainty.3
Total costs were calculated from the healthcare as well as the societal perspective. Values were discounted using a discount rate of 4% per year for costs, and 1.5% for QALYs according to Dutch guidelines for economic evaluations in healthcare.2
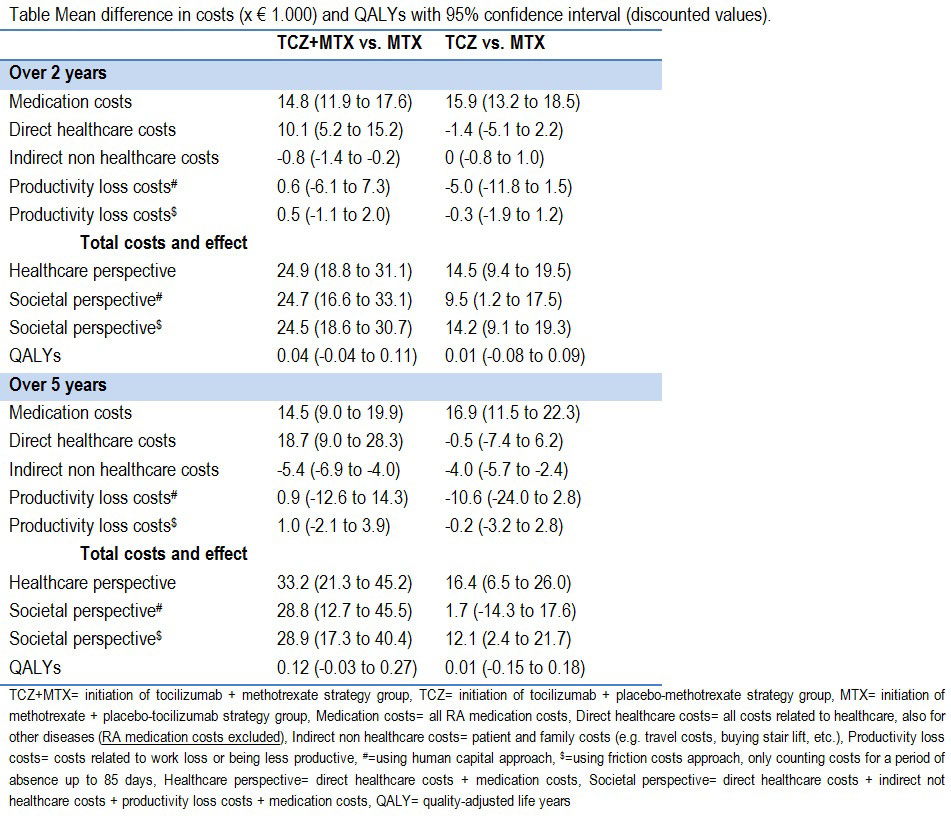
Differences in costs and QALYs were calculated for TCZ+MTX vs. MTX and TCZ vs. MTX over a 2 year and 5 year time horizon. Cost-effectiveness acceptability curves were constructed to illustrate the probability of TCZ(+MTX) being cost-effective at different willingness to pay (WTP) thresholds.
Results: Approximately 80% of all patients were employed at baseline, and worked on average 24 hours weekly without differences between strategy groups.
Differences in costs per category (i.e. costs for medication, direct healthcare, indirect non healthcare, and productivity loss) and QALYs are shown in the Table. Differences in QALYs increased between 2 and 5 years, without becoming statistically significant. In most cost categories, no differences were observed either over 2 or 5 years. Medication costs were, as expected, higher in the treatment strategies initiating TCZ. Savings were made in indirect non healthcare costs for TCZ+MTX and TCZ respectively, and productivity loss costs were numerically lower for TCZ. The probability of TCZ(+MTX) being a cost-effective intervention over 5 years, using different WTP thresholds for a QALY, was in general low, and somewhat higher for TCZ compared to TCZ+MTX, see Figure.
Conclusion: Based on current analyses, early initiation of TCZ, with or without MTX, is not cost-effective compared to MTX initiation in a step-up treat-to-target treatment strategy over 2 or 5 years in early RA patients. However, these outcomes are based on limited data.
Reference
- Bijlsma JWJ, et al. Lancet. 2016;388:343-355.
- Zorginstituut Nederland. 2016;1-120.
- Brand J, et al. Stat Methods Med Res. 2019;38:210-220.
To cite this abstract in AMA style:
Verhoeven M, Tekstra J, Pethö-Schramm A, Borm M, van Laar J, Lafeber F, Bijlsma J, Jacobs J, Welsing P. Impact on Costs and Quality of Life over 5 Years of Treat-to-target Treatment Strategies Initiating Tocilizumab, Methotrexate or Their Combination in Early Rheumatoid Arthritis: Economic Evaluation of the U-Act-Early Trial [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/impact-on-costs-and-quality-of-life-over-5-years-of-treat-to-target-treatment-strategies-initiating-tocilizumab-methotrexate-or-their-combination-in-early-rheumatoid-arthritis-economic-evaluation-of/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-on-costs-and-quality-of-life-over-5-years-of-treat-to-target-treatment-strategies-initiating-tocilizumab-methotrexate-or-their-combination-in-early-rheumatoid-arthritis-economic-evaluation-of/