Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
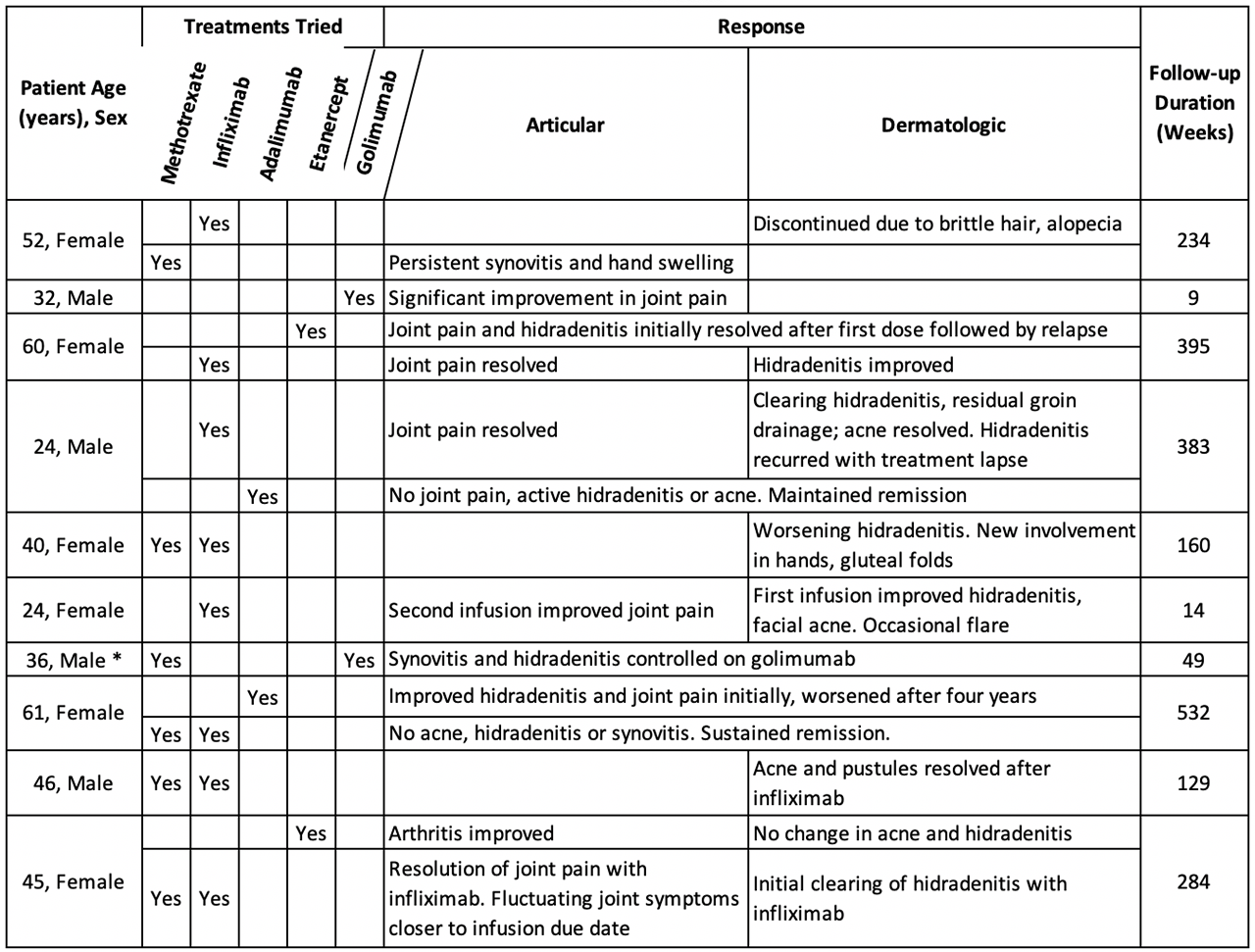
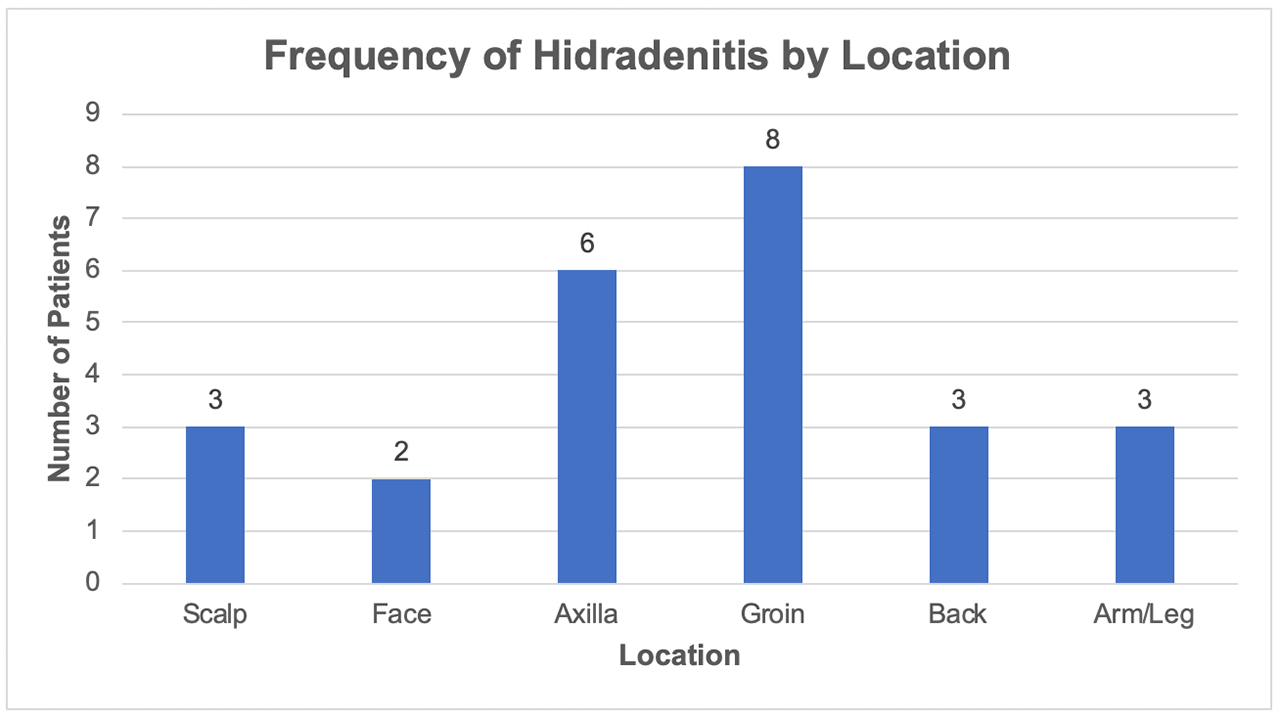
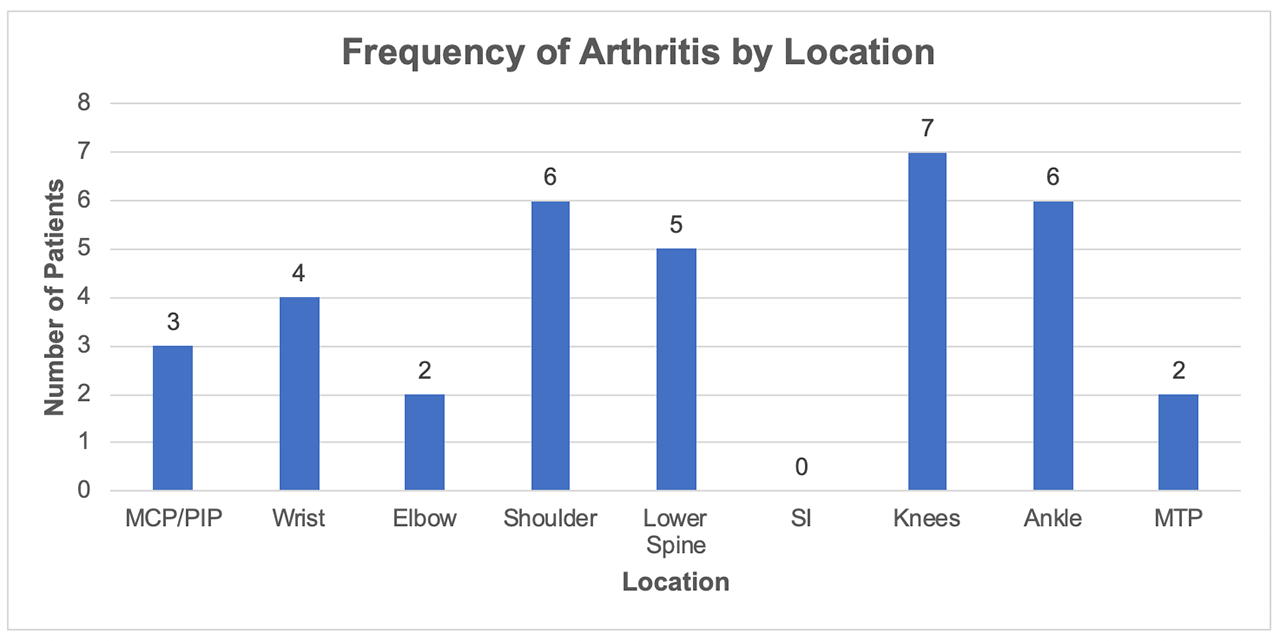
Background/Purpose: SAPHO is a chronic multisystemic illness with predominantly skin and joint manifestations. Disease presentation is heterogenous; proposed diagnostic criteria include chronic multifocal aseptic osteomyelitis and osteitis of the long bones1,2. Due to SAPHO’s rarity, treatment is based on observational studies and case reports. Anti-TNF therapy is increasingly used in refractory SAPHO cases. We present a series of 10 patients diagnosed with SAPHO and their response to various anti-TNF agents.
Methods: We performed a retrospective single-center study of SAPHO patients on anti-TNF therapy followed by rheumatology and dermatology from 2014 to 2017. Patients 18 or older were screened for SAPHO using ICD-10 codes for hidradenitis suppurativa, acne vulgaris, pustulosis, palmar pustulosis, palmoplantar pustulosis, AS, inflammatory spondylopathy, seronegative SpA, and inflammatory arthritis in combination. Patients were excluded if an alternate diagnosis was made, lost to follow-up, or did not start anti-TNF therapy. We identified 10 SAPHO patients treated with TNF inhibitors and characterized their articular and dermatologic responses.
Results: 10 patients (6 female, 4 male) with a mean age of 38 years (range 19-52) were followed for an average period of 50 months (range 2–122). 6 of the 10 patients (60%) had prior MTX or bisphosphonate use. Infliximab was used in 8 patients of whom 6 had significant improvement in pustulosis and joint pain while 2 patients experienced worsening symptoms. 4 patients (40%) required two or more anti-TNF agents. The average ESR and CRP were 32 mm/hr and 5.8 mg/L at the outset and 26 mm/hr and 2.52 mg/L at the end of therapy, respectively.
Conclusion: Anti-TNF therapy is effective in treating cutaneous and articular manifestations of refractory SAPHO. Infliximab was most widely used in our study and associated with marked improvement in acne, pustulosis and arthritis. Etanercept was less effective in treating skin than articular disease. Golimumab and adalimumab showed similar clinical response. At present, a lack of validated response criteria specific for SAPHO limits objective assessment of therapeutic response. Further research is needed to better gauge response to therapy.
To cite this abstract in AMA style:
Verma D, Shah S, Jayatilleke A. Synovitis, Acne, Pustulosis, Hyperostosis, and Osteitis (SAPHO): A Case Series [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/synovitis-acne-pustulosis-hyperostosis-and-osteitis-sapho-a-case-series/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/synovitis-acne-pustulosis-hyperostosis-and-osteitis-sapho-a-case-series/