Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Hidradenitis Suppurativa (HS) is an inflammatory disease of the apocrine sweat glands characterized by recurrent abscessing inflammation. The molecular drivers of HS are poorly understood, but smoking is strongly associated with disease activity. The US Food and Drug Administration (FDA) recently approved tumor necrosis factor-alpha inhibitors (TNF-i) for HS. However, little is known about the relationship between smoking and remission rates in patients receiving TNF-i therapy for HS. The purpose of this study was to investigate the relationship between smoking and HS remission rates in a longitudinal cohort of patients receiving ongoing therapy for HS.
Methods: This study was conducted through the Wound Etiology and Healing Study (WE-HEAL Study), an IRB approved biospecimen and data repository for tracking outcomes in HS. All subjects gave written informed consent for longitudinal collection of their data while they received treatment according to standard of care. Demographic data, baseline medical comorbidities, smoking and disease activity scores were collected. Patients were categorized by smoking status at last follow up (current, never, past). Disease activity was assessed using Hurley Stage, Hidradenitis Sartorius Score (HSS), and Active Nodule (AN) Count. Remission was a binary outcome based on achieving the Hidradenitis Suppurativa Clinical Response (HiSCR). Statistical analysis was conducted using SAS version 9.4. Multivariable Cox proportional hazard model was used for analysis.
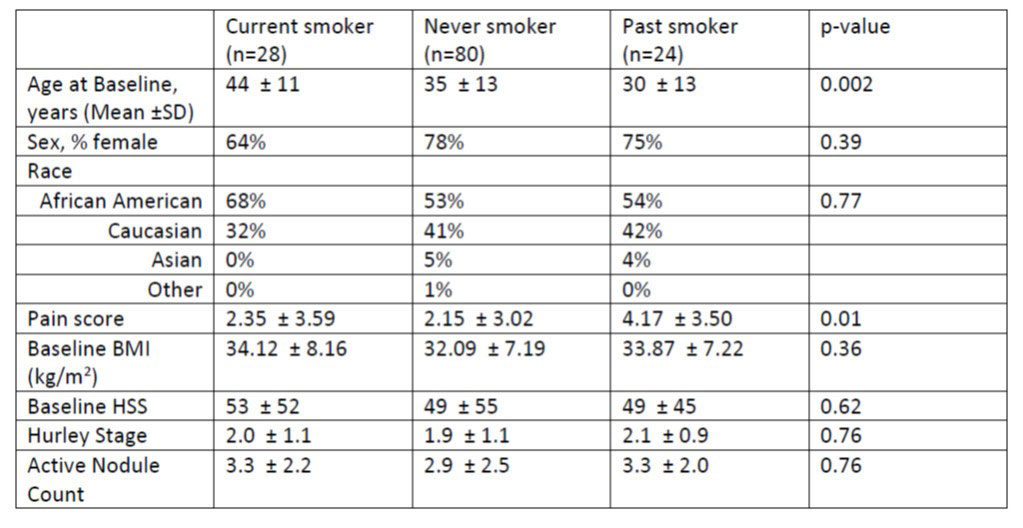
Results: At the time of data lock, there were 132 patients in the WE-HEAL HS cohort: current smokers (21%), past smokers (18%), never smokers (61%). There was no statistically significant difference between the groups in regards sex, race or baseline body mass index (BMI). The past smoker group had a higher baseline pain score (p=0.01) and current smokers tended to be slightly older (p=0.002). There was no significant difference between the three groups in baseline disease activity scores (Table 1).
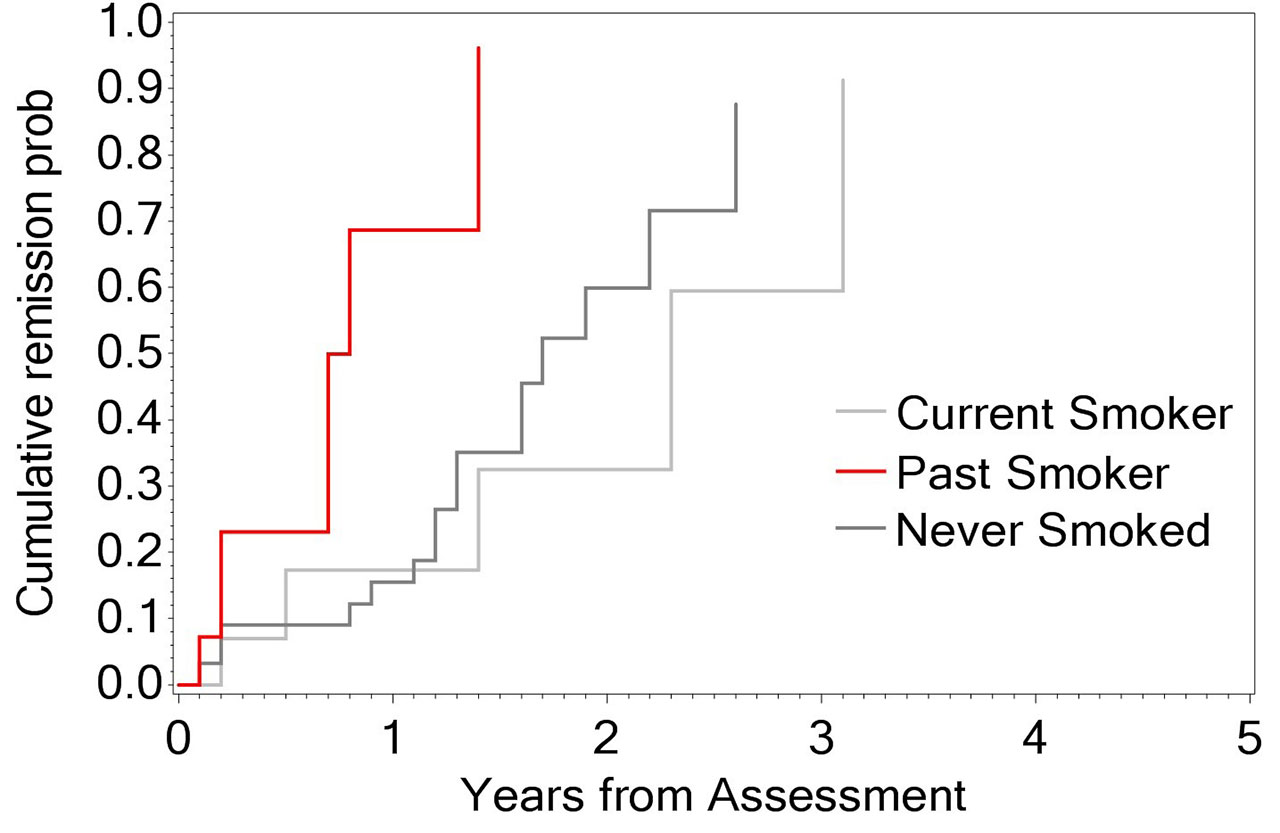
Time to remission did not differ significantly between smoking categories in univarible KM analysis (log-rank p = .18). However, after adjusting for age, ever receiving MTX, TNFi, or opioids, and ever having HS surgery, the HR for current smoker vs past smoker reaching remission is 0.31 (0.10-0.98) (p=.046). This indicates that past smokers reach remission more quickly than current smokers (Figure 1). Never-smoked differed from past-smoker only at a trend level of significance (aHR 0.43 [0.18-1.04], p=.06). The only other covariate associated with remission was ever receiving opioids. Those who did receive opioids had reduced likelihood of reaching remission (aHR 0.24 [0.08-0.72], p=.01).
Conclusion: The current analysis shows that patients who continue to smoke demonstrate lower and slower rates of achieving remission than those who stop smoking or never smoked. This data not only supports the strong benefit of smoking cessation in HS management, but also suggests that smoking may impact the immune drivers of HS.
To cite this abstract in AMA style:
Agarwal A, Mangini M, Jones D, Hood C, Amdur R, Shanmugam V. Impact of Smoking Status on Remission in Hidradenitis Suppurativa [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/impact-of-smoking-status-on-remission-in-hidradenitis-suppurativa/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-smoking-status-on-remission-in-hidradenitis-suppurativa/