Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: All providers, including rheumatologists, spend approximately half of their day documenting in an electronic health record (EHR). Excessive documentation is a key contributor to burnout, which is associated with reduced quality of care and poor patient satisfaction. We performed a quality improvement project to increase documentation efficiency in an academic rheumatology practice.
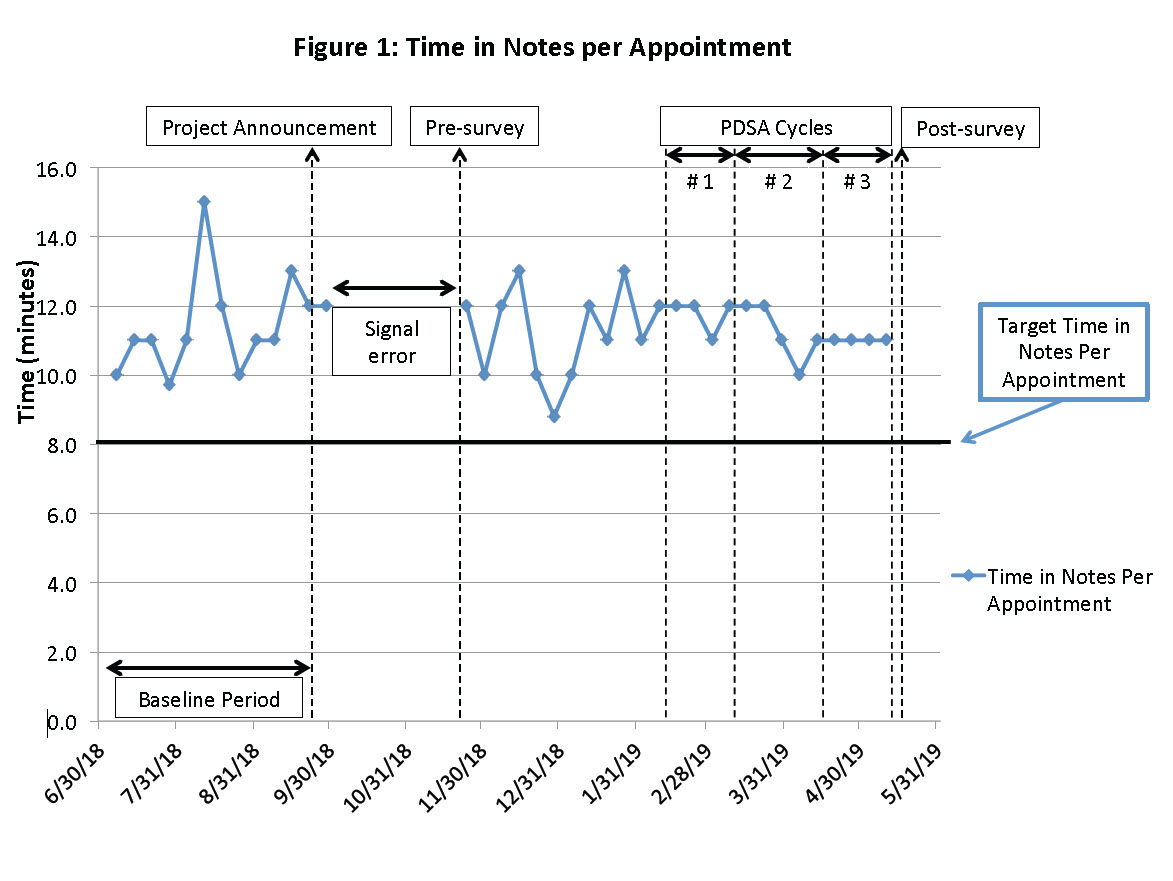
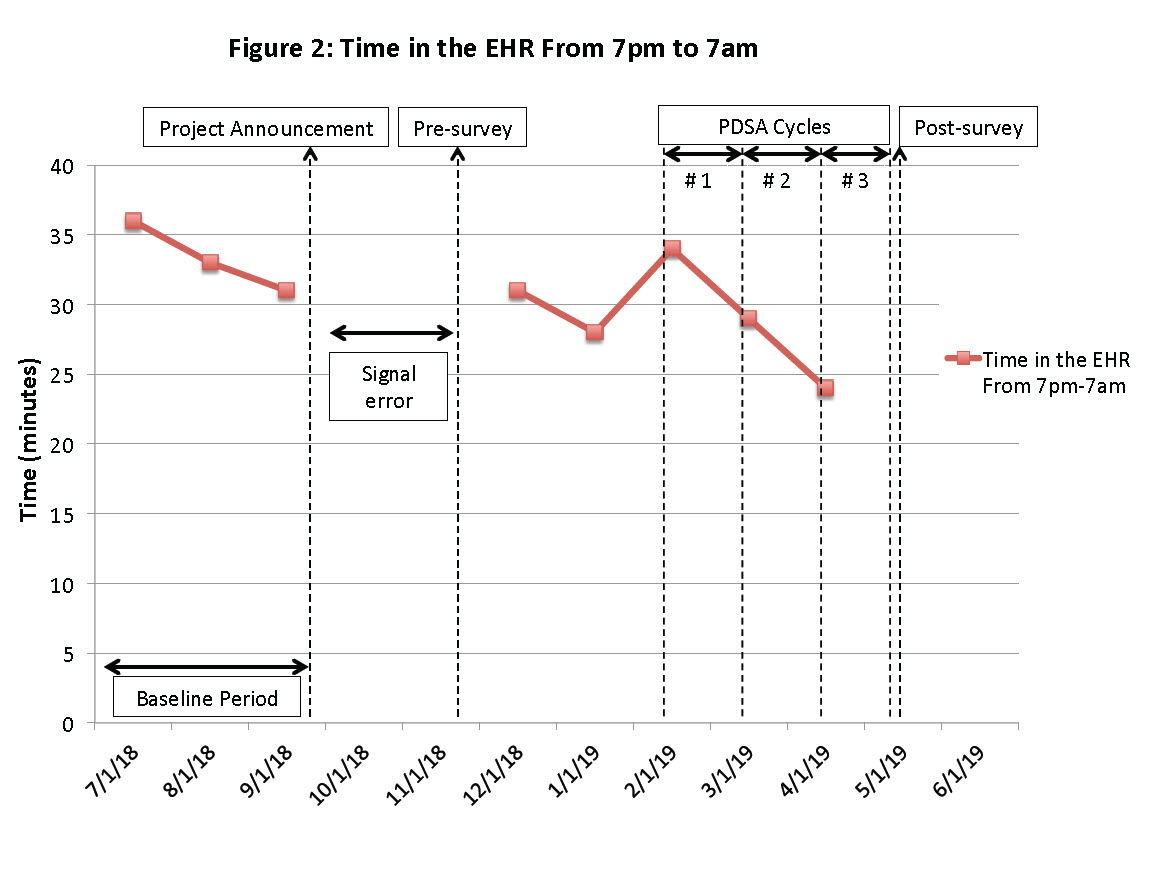
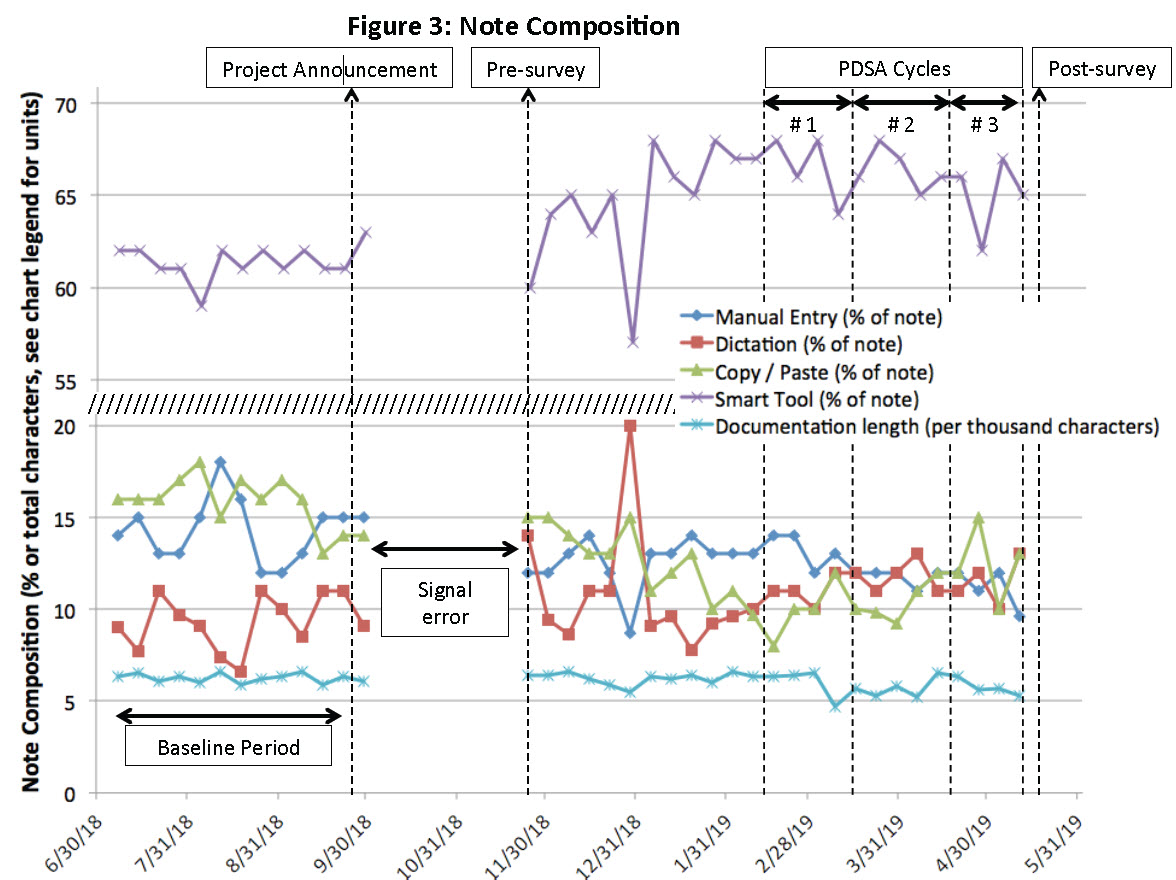
Methods: We used Signal, an Epic analytic data tool, to obtain documentation performance metrics. Our primary aim was to reduce average “time in notes per appointment” from over 10 min to 8 min (Epic’s nationwide rheumatology average). Secondary measures included average time in the EHR from 7pm-7am and note composition metrics. To assess need and impact, we distributed a pre and post-survey to providers in our practice regarding their documentation practices, satisfaction with documentation time, and engagement with interventions. Using Plan-Do-Study-Act (PDSA) methodology, we conducted these cycles: (1) dictation training, (2) a presentation on recommendations to increase efficiency, and (3) optional individual training sessions with EHR experts. Signal data was recorded weekly except for 7pm-7am time, which was recorded monthly. Data is analyzed using descriptive statistics.
Results: Average “time in notes per appointment” was 11.4 min at baseline, 12 min after PDSA1, 11 min after PDSA2, and 11 min after PDSA3 (Figure 1). Average time in the EHR from 7pm-7am was 33.3 min at baseline vs. 29 min after PDSA1 and 24 min after PDSA2, data pending from PDSA3 (Figure 2). Average note composition percentages at baseline vs. after PDSA1, 2, and 3 were: manual entry 14.3 vs. 12, 12, and 9.6%; dictation 9.3 vs. 12, 11, and 13%; copy/paste 15.9 vs. 10, 12, and 13%; smart tool 61.3 vs. 66, 66, and 65%. Average documentation length was 6.25K characters at baseline vs. 5.7K, 6.5K and 5.3K (Figure 3). Twenty-five of 27 (93%) providers responded to both the pre and post-surveys. Satisfaction with documentation time on the pre- vs. post-survey was: “completely” or “very dissatisfied” 44% vs. 32%; “dissatisfied” 40% vs. 40%; and “satisfied” 16% vs. 28%. Respondents wrote notes from home “often” or “almost always” in 60% vs. 37.5%. Missing out on activities outside of work in order to finish notes occurred “often” or “almost always” for 24% vs. 12.5%. Regarding engagement with interventions, 32% of post-survey respondents reported newly using dictation software, 36% increased their use of dictation, and 52% modified note templates.
Conclusion: Though we did not meet our aim of reducing average time in notes per appointment, interventions led to providers using more dictation and smart tools with a corresponding reduction in manual data entry. Perhaps most importantly, both Signal and survey data suggested that providers spent less time in the EHR at home after our interventions; the percentage reporting missing out on activities outside work to document dropped by half. Practice-wide focus on improving documentation efficiency led to improved satisfaction with the documentation process and enabled providers to enjoy more activities outside of work. Future measurement targets may include care quality and burnout metrics.
To cite this abstract in AMA style:
Leverenz D, Golenbiewski J, Andonian B, Kaufman K, Chu P, Maheswaranathan M, Johannemann A, Doss J, Criscione-Schreiber L. A Quality Improvement Project to Increase Documentation Efficiency in an Academic Rheumatology Practice [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/a-quality-improvement-project-to-increase-documentation-efficiency-in-an-academic-rheumatology-practice/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-quality-improvement-project-to-increase-documentation-efficiency-in-an-academic-rheumatology-practice/