Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: High risk of premature cardiovascular disease (CVD) among SLE patients is well documented, but the best means to detect the earliest stages of CVD in SLE are not known. Coronary microvascular dysfunction is thought to be one of the earliest detectable abnormalities and can be detected by measuring coronary flow reserve (CFR) with positron emission tomography (PET) scanning. PET-CFR is an emerging prognostic imaging technique used to detect increased CVD risk including death in non-SLE populations, even among those without overt obstructive coronary artery disease. We aimed to measure coronary microvascular function by CFR in active SLE patients and to compare findings to those of patients with diabetes mellitus (DM) and non-SLE, non-DM controls.
Methods: We identified SLE patients with active disease (SLE disease activity index > 6), internal organ involvement and no history of known coronary artery disease, followed at the Brigham and Women’s Hospital Lupus Center. Pre-menopausal women and similar aged female controls without SLE or DM were enrolled as comparisons. Demographic and clinical data were collected. All subjects underwent rest and then stress myocardial perfusion PET scans, from which we measured regional and global left ventricular myocardial blood flow (in mL/min/g of tissue) and calculated the CFR as the ratio of myocardial blood flow during stress to that at rest. We used t-tests and Chi-squared tests to compare subject demographic characteristics, and ANOVA tests to compare mean global myocardial blood flow and CFR values between SLE, DM and control subjects.
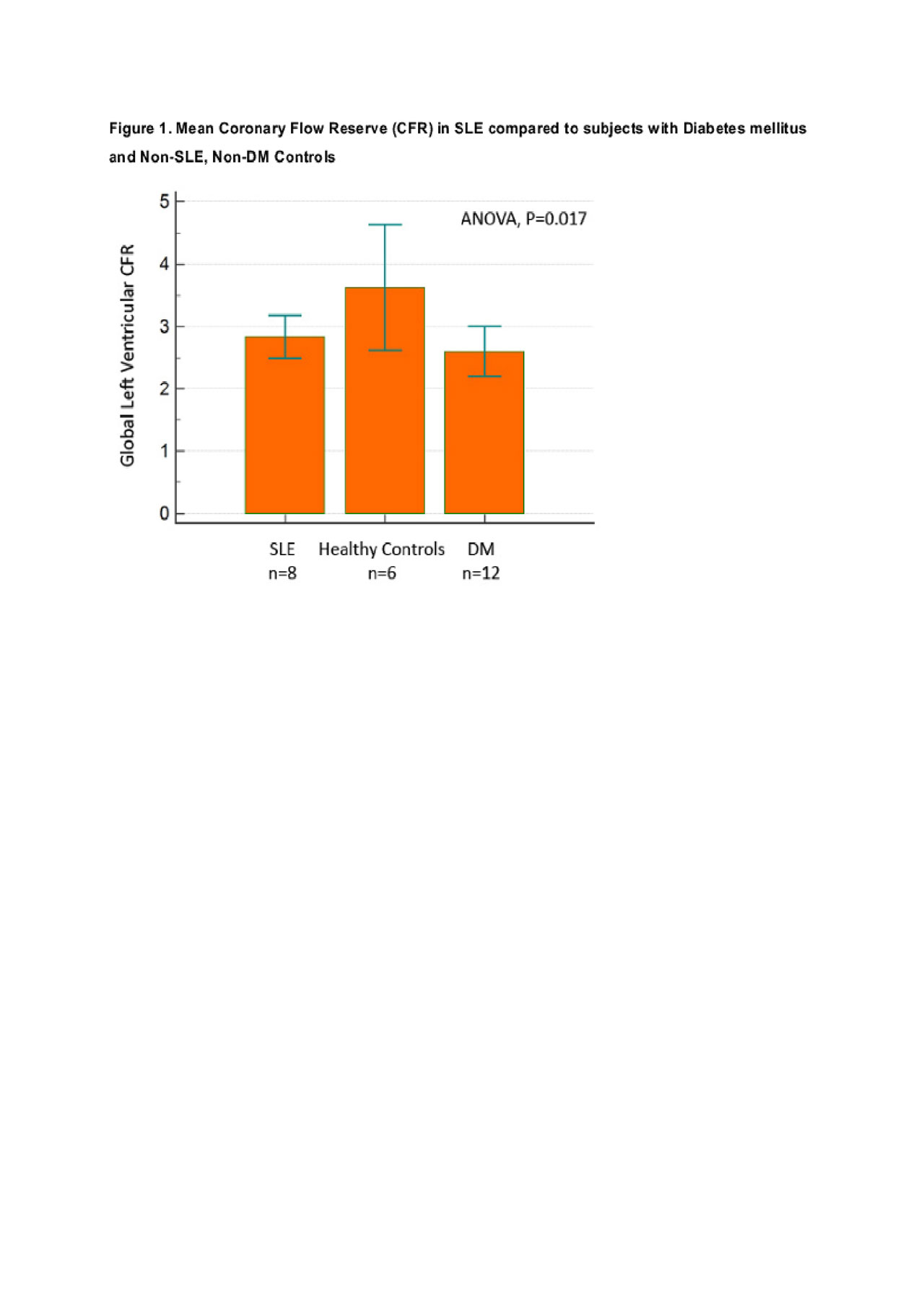
Results: We studied 8 SLE, 12 DM and 6 control female subjects, all with normal PET scans indicating no evidence of obstructive CAD. Demographics are shown in Table 1. All SLE subjects were anti-dsDNA positive, 5/8 had lupus nephritis, and their mean SLEDAI score was 10 (SD 4.5) (Table 1). Rest myocardial blood flow was comparable across the three groups. Adenosine-stimulated myocardial blood flow was similar in SLE and pre-menopausal diabetic women (2.64 ± 0.52), but 21% lower in SLE patients than in controls (2.44 ± 0.28 vs. 3.09 ± 0.32 mL/min/g, p< 0.05) (Table 2). Although SLE patients were younger than the pre-menopausal DM women, they showed similar reduction in global CFR (Figure 1). Compared to controls, subjects with active SLE had a 22% reduction in global CFR (2.84 ± 0.41 vs 3.63 ± 0.96, p< 0.05).
Conclusion: Subjects with active SLE had a significant reduction in coronary microvascular function compared to non-diabetes, non-SLE controls. This reduction was similar to that observed in slightly older premenopausal women with diabetes mellitus. These preliminary findings suggest that coronary microvascular dysfunction, likely driven by inflammation in active SLE, may be an early marker of CVD risk among SLE patients, as it is in DM patients. Although studies are needed, PET-CFR may prove to be a useful tool for stratifying SLE patients in terms of their risks of CVD events and death.
We thank the John J. Holland and Virginia M. Bruen Fund for Systemic Lupus Erythematosus Research for supporting this study.
To cite this abstract in AMA style:
Speyer C, Sinnette C, Stevens E, Guan H, Bibbo C, Di Carli M, Costenbader K, Massarotti E. Novel PET-Coronary Flow Reserve Imaging to Assess for Coronary Microvascular Dysfunction in Systemic Lupus Erythematosus Compared to Subjects with Diabetes Mellitus and Controls [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/novel-pet-coronary-flow-reserve-imaging-to-assess-for-coronary-microvascular-dysfunction-in-systemic-lupus-erythematosus-compared-to-subjects-with-diabetes-mellitus-and-controls/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/novel-pet-coronary-flow-reserve-imaging-to-assess-for-coronary-microvascular-dysfunction-in-systemic-lupus-erythematosus-compared-to-subjects-with-diabetes-mellitus-and-controls/