Session Information
Date: Monday, November 11, 2019
Title: Epidemiology & Public Health Poster II: Spondyloarthritis & Connective Tissue Disease
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Non-steroidal anti-inflammatory drugs (NSAIDs) and opioids are prescribed for the management of pain among patients with rheumatic diseases including systemic lupus erythematosus (SLE). However, both types of medication can be associated with serious side effects. For example, increased mortality has been reported among people who use opioids. Our purpose in this study was to describe the trends in prescribing of NSAIDs (including coxibs) and opioids among patients with SLE in the general population.
Methods: We use a population-based administrative database that included all prescriptions for persons aged 20+ processed by pharmacies in the entire province, between 1998 and 2014, linked to diagnostic codes for visits to physicians and hospitalizations. We identified all prevalent cases of SLE, defined as at least 2 codes at least 2 months apart within 2 years. We identified all prevalent prescriptions for each NSAID and opioid available in the province and calculated the proportion of people receiving NSAID or opioid medication.
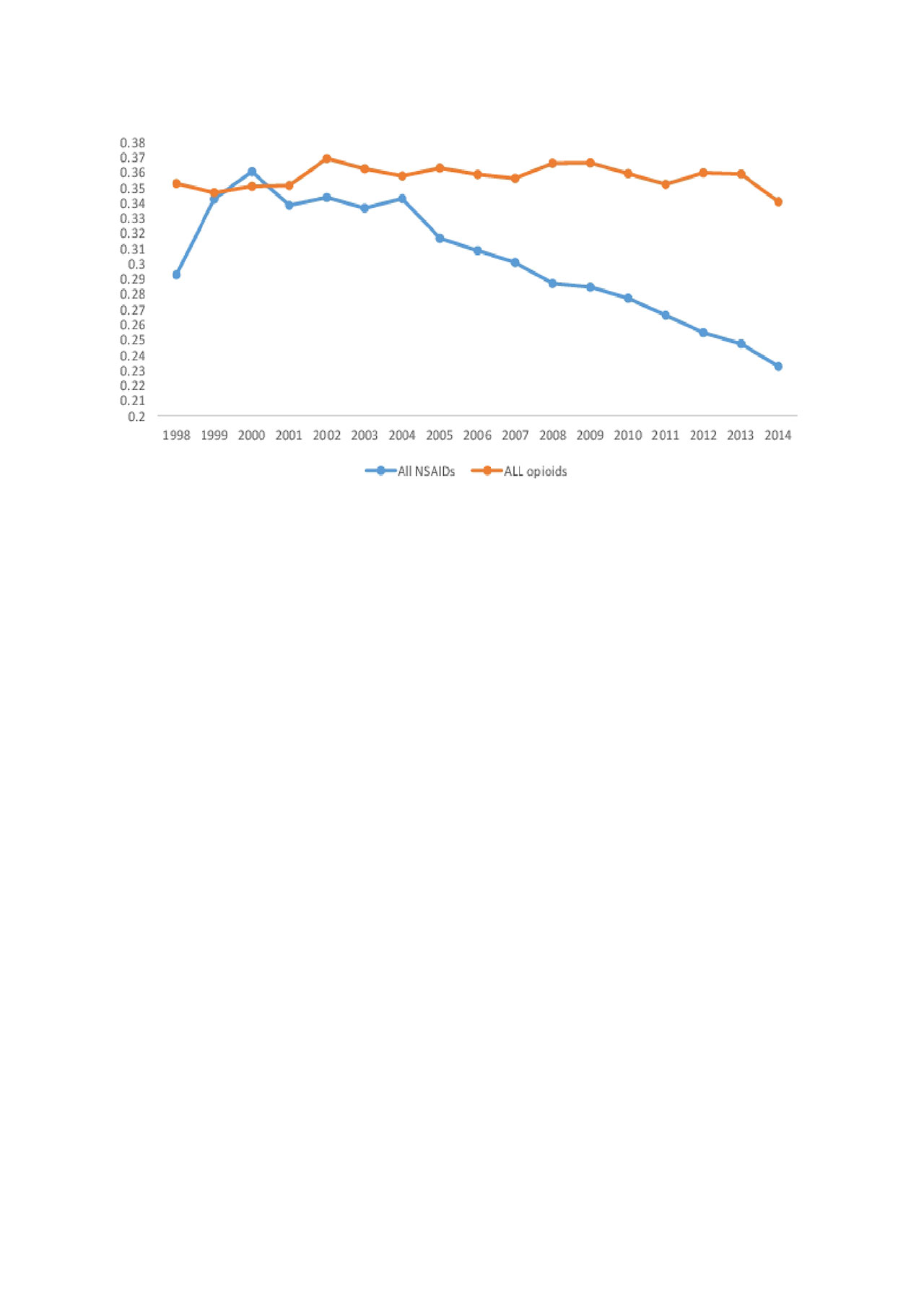
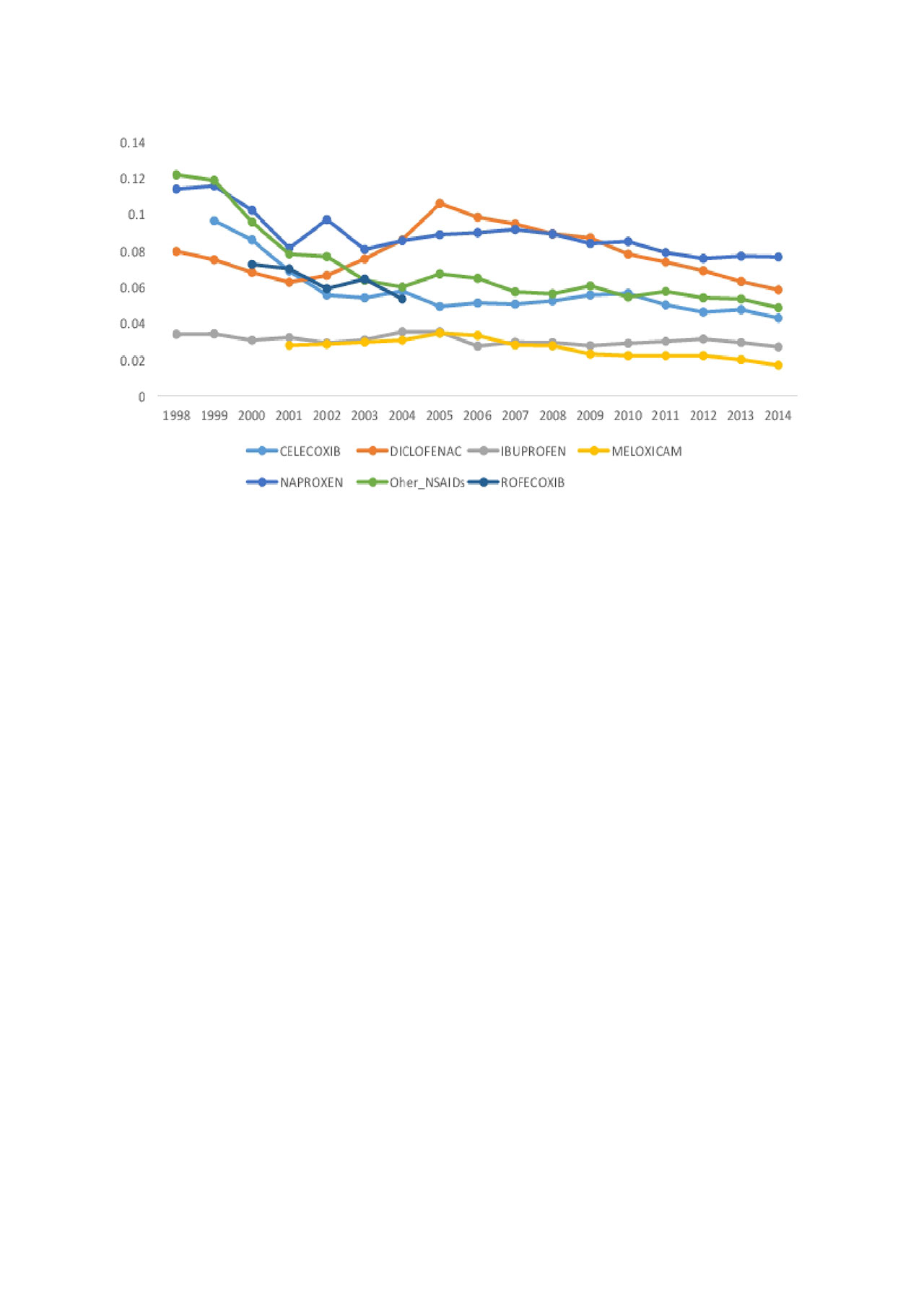
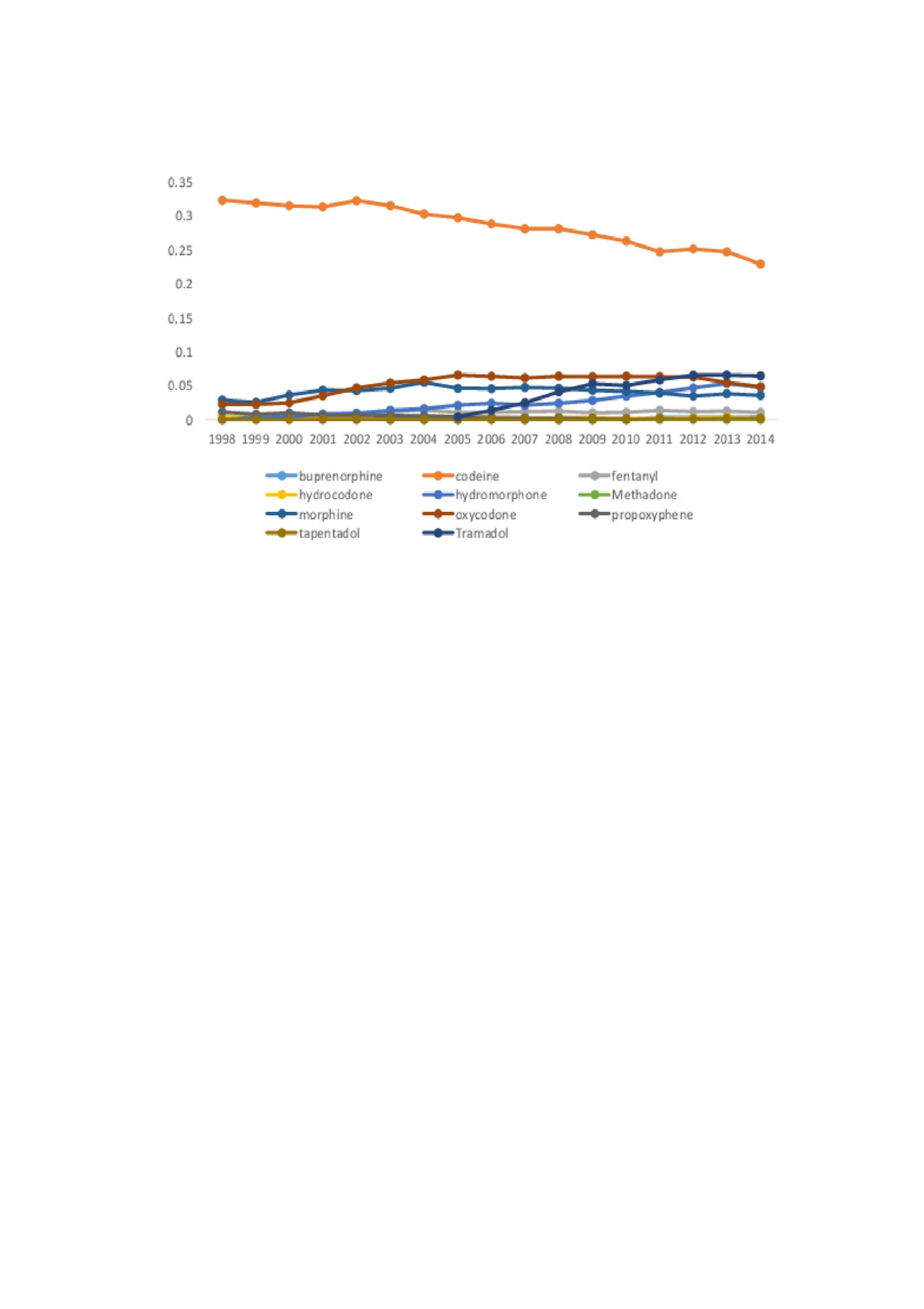
Results: Between 1998 and 2014, the proportion of SLE patients with an NSAID prescription declined from 29.2% to 23.2% (Figure 1). For most NSAIDs (Figure 2), prescriptions declined aggressively as of 2004 and were relatively stable until 2014, with the exception of diclofenac, which increased substantially from 2001 to 2005 and decreased afterwards. In 2014, the most common NSAID was naproxen (7.7%) followed by diclofenac (5.8%), celecoxib (4.3%), ibuprofen (2.7%) and meloxicam (1.7%). For opioids (Figure 1), the overall trend was relatively flat from 1998 to 2014, with 35.3% in 1998 to 34.1% in 2014. Codeine was by far the most commonly prescribed opioid throughout the study period, but declined from 32.2% of prevalent SLE patients in 1998 to 22.8% in 2014 (Figure 3). Tramadol increased steadily from its introduction in 2005 and has been the second most common opioid since 2012, reaching 6.4% in 2014. Prescriptions for oxycodone started to decline around 2011 and reached 4.8% in 2014, whereas those for hydromorphone steadily increased (4.7% in 2014). Morphine increased slightly from 1998, reaching 5.5% in 2004, then declined thereafter. Other opioids were rarely prescribed in patients with SLE.
Conclusion: There have been important changes in the pattern of prescribing analgesics in our province during the study period. Declines in NSAIDs may have been compensated by increased prescriptions for some opioids. This is likely to change as new guidelines discourage the long-term use of opioids as a consequence of the current opioid crisis.
To cite this abstract in AMA style:
Li L, Lu N, Kopec J, Esdaile J, Xie H, Avina-Zubieta J. Trends in NSAIDs and Opioids Among Patients with SLE: A Population-based Study [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/trends-in-nsaids-and-opioids-among-patients-with-sle-a-population-based-study/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/trends-in-nsaids-and-opioids-among-patients-with-sle-a-population-based-study/