Session Information
Date: Sunday, November 10, 2019
Title: 3S089: Health Services Research I: Clinical Perspectives (951–956)
Session Type: ACR/ARP Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Medicare measures readmissions within 30 days of hospitalization across several conditions as a marker of care quality. While not currently a reporting condition, in systemic lupus erythematosus (SLE) observed 30-day readmission rates range from 17-27%, rivaling reportable conditions such as congestive heart failure (CHF). No controlled studies thus far have performed such between-condition comparisons. Using a nationwide Medicare cohort, we compared adjusted readmission rates among SLE, CHF, and the general Medicare population, and assessed relationships between patient and hospital factors and 30-day readmissions in SLE with the goal of identifying targets for readmission prevention measures.
Methods: Using claims data from a 20% random US national Medicare sample, we identified all patients with inpatient hospitalizations in 2014 to compare risk of 30-day readmission among patients with SLE to those with CHF and the general Medicare population. Inclusion required age of at least 18 years old, live discharge, and at least 12 months of continuous Medicare part A and B coverage prior to index admission. Baseline patient and hospital covariates included age, sex, race, ethnicity, Medicaid, baseline year comorbidity, prior hospitalization, hospital volume, medical school affiliation, and area deprivation index (ADI)–a measure of neighborhood disadvantage from patients’ census block group. Analysis used multivariable Cox proportional-hazards regression clustered by patient to find adjusted hazard ratios (HRs) of 30-day readmission among patients with SLE compared to those with CHF and the general Medicare population.
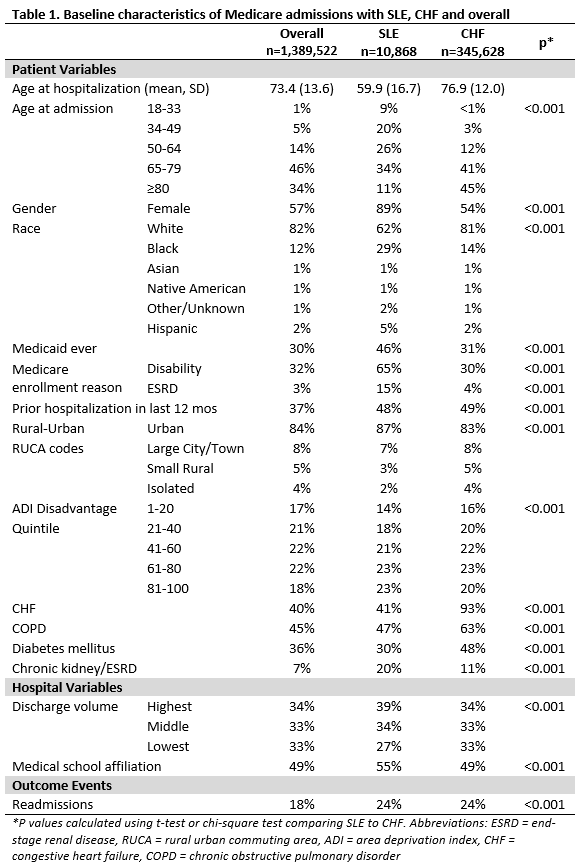
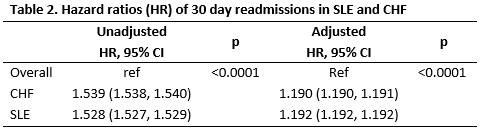
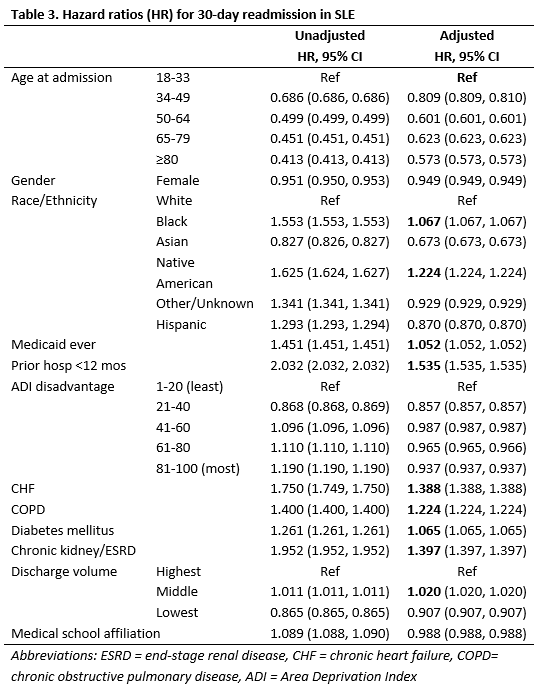
Results: The SLE cohort (n=10,868) was younger by nearly 20 years and predominantly female. They were twice as likely to be Black, on Medicaid or disabled, and had nearly four-fold higher ESRD as compared to CHF or general Medicare (Table 1). The 30-day readmission rate of 24% was identical for SLE and CHF, and significantly higher than the general Medicare cohort rate of 18%. Patients with CHF and SLE had similarly elevated hazard ratios for readmission (HR 1.190, 95% CI 1.190, 1.191 and HR 1.192, 95% CI 1.192, 1.192, respectively; Table 2), compared to patients without either condition. Among patients with SLE, readmission risk was highest in the 18-33 age group (Table 3). Higher readmission risk was also observed in SLE patients who were Black, Native American, hospitalized within the past year, and who had comorbidities including CHF, COPD, and ESRD. Dual Medicaid status predicted slightly increased risk, and hospital factors were more modestly predictive. Overall, primary diagnoses for readmissions did not significantly differ between groups.
Conclusion: 30-day readmission rates in SLE are as high as those in CHF, with readmissions impacting one in four hospitalized SLE patients. Transitional care programs, Medicare policies, and other efforts designed to reduce readmissions should consider focusing on SLE, a high risk group for readmissions that is currently not widely recognized as such. Existing interventions should particularly target SLE patients who are younger, with ESRD or prior hospitalization.
To cite this abstract in AMA style:
Chodara A, Wang X, Shi F, Garg S, Powell R, Schletzbaum M, Sheehy A, Kind A, Bartels C. Rate of Thirty-Day Readmissions in Systemic Lupus Erythematosus Rivals Congestive Heart Failure and Exceeds the General Medicare Population [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/rate-of-thirty-day-readmissions-in-systemic-lupus-erythematosus-rivals-congestive-heart-failure-and-exceeds-the-general-medicare-population/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rate-of-thirty-day-readmissions-in-systemic-lupus-erythematosus-rivals-congestive-heart-failure-and-exceeds-the-general-medicare-population/