Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Chronic pain is a complicated issue that has received a significant amount of attention. In particular, studies suggesting the role of central sensitization in chronic pain conditions, have supported the utility of centrally acting agents in the management of these conditions. Duloxetine, a selective serotonin and norepinephrine reuptake inhibitor, has central nervous system activity and has been has been approved for these syndromes. It was initially approved in 2004 for treatment of depression and neuropathic pain. In 2008, it use extended to the management of FMS and in 2010 to the treatment of chronic musculoskeletal pain, including OA. The utility of this agent in the “real world” is not clear. Here, we evaluated the trends of duloxetine use in a tertiary care rheumatology practice for chronic pain conditions, with emphasis on length of therapy and improvement in patient-reported outcomes.
Methods: IRB approval was obtained. A single center retrospective study was performed of patients with ICD-10 diagnoses of OA, chronic pain syndromes and FMS who were prescribed duloxetine between 2010 and 2019. Age, sex, ethnicity, dose of medication, length of use and multidimensional health assessment questionnaire (MDHAQ) scores pre and post treatment were recorded. Individuals with any diagnosis of mood disorder were excluded. Chi squared and paired t tests were used to analyze differences in prescribing patterns and improvement in patient reported outcomes.
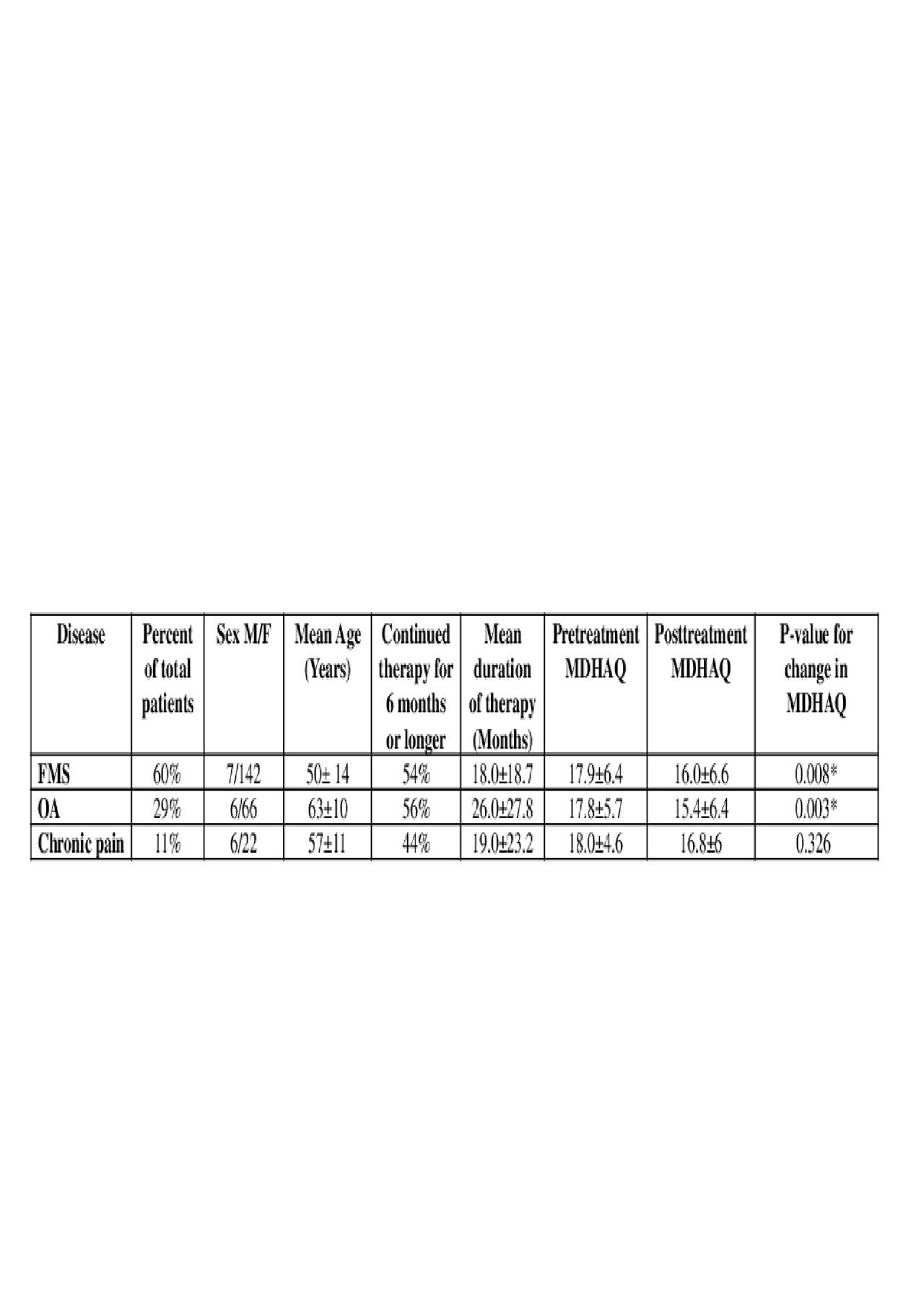
Results: Of 1700 charts reviewed, 250 met inclusion criteria. Of the patients being prescribed duloxetine, 149 had a primary diagnosis of FMS, 71 had OA and 28 had chronic pain. Results are summarized in the Tables. MDHAQ scores significantly improved with duloxetine use in FMS and OA groups, however there was no significant improvement in scores in the chronic pain group . In addition, there was significant improvement of MDHAQ scores in Caucasian and African American patients prescribed duloxetine, while this improvement was not observed in Hispanics patients. Duloxetine 30 mg daily was the most frequently prescribed dose in each condition. In total, over 54% of the patients continued therapy for over 6 months, with a mean duration of therapy in those that continued as high as 26 months in the OA group. In addition, our data suggest that physicians in practice for over 15 years prescribed more duloxetine compared to those in practice less than 15 years (p< 0.03).
Conclusion: The results of the current study are supportive of previous clinical trial studies in that patient reported outcomes improve significantly during the period of use of duloxetine. Although this improvement cannot directly be attributed to medication use alone, its potential efficacy is also supported by the continued use of the medication for an extended period of time. Chronic pain syndrome patients did not demonstrate significant improvements, however this may be limited by the small number of patients. Interestingly, improvements varied by ethnicity, and these differences could be evaluated in future studies. Finally, considering differences in prescribing based on years in practice, education for younger professionals on the potential utility of this drug may be warranted.
To cite this abstract in AMA style:
Shastri R, Khandelwal S, Shakoor N. Duloxetine for Chronic Pain Management in a Tertiary Care Rheumatology Practice: How Patients Are Doing in the Real World [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/duloxetine-for-chronic-pain-management-in-a-tertiary-care-rheumatology-practice-how-patients-are-doing-in-the-real-world/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/duloxetine-for-chronic-pain-management-in-a-tertiary-care-rheumatology-practice-how-patients-are-doing-in-the-real-world/