Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with comorbid fibromyalgia syndrome (FMS) and bipolar disorder (BD) were found to have more severe FMS. The Mood disorders questionnaire (MDQ), a self-reported inventory of lifetime history of manic and hypomanic symptoms has been proposed as a screening tool for BD, but its specificity for BD has been controversial. We evaluated the relationship between MDQ and a history of self-reported prior clinical diagnosis of BD.
Methods: Consecutive patients diagnosed clinically with FMS were enrolled and demographic, socioeconomic and clinical data were collected. Patients completed the following standardized questionnaires; for depression PHQ-9 (patient health questionnaire), anxiety GAD-7 (generalized anxiety disorder questionnaire), disability HAQ-DI (health assessment questionnaire disability index), PDI (pain disability index), PSD (polysymptomatic distress scale/fibromyalgianess scale), WPI (widespread pain index), SS (symptom severity scale), FIQ (fibromyalgia impact questionnaire).
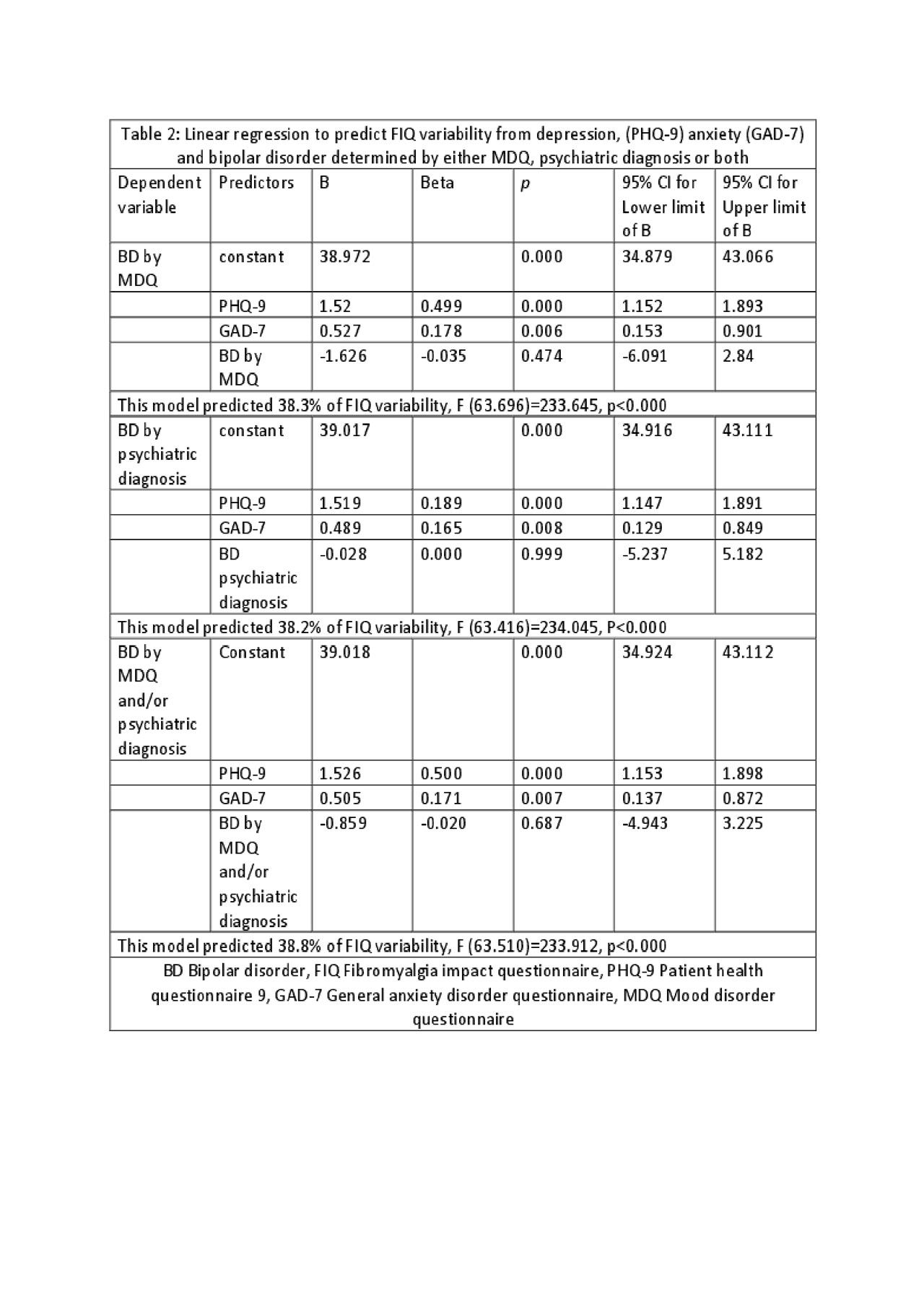
Results: We enrolled 430 patients with FMS who completed the MDQ and also reported a history of psychiatric evaluation, of which 118 (27.5%) had bipolar disorder by either MDQ or prior psychiatric diagnosis. The mean age was 43.3 (12.0), 89.3% female and 87.7% met the ACR 2010 criteria for FMS. The mean MDQ was 3.9 (3.3) and 20.9% had an MDQ >=7. A psychiatric diagnosis of BD was made in 59 (13.7%) of patients; 6.7% (29%) had a BD diagnosis by psychiatry and an MDQ of < 7. Thirty patients (7%) had a diagnosis of BD both by MDQ and psychiatry. Correlation between MDQ and a past psychiatric diagnosis of BD was low, r= 0.293 (p< 0.005). The sensitivity of an MDQ ³7 for a prior diagnosis of BD was 42.4% and the specificity was 13.5%. Patients with MDQ³ 7 had significantly higher scores on depression and anxiety as well as higher fibromyalgianess, fibromyalgia severity and disability scores (Table 1). We performed three separate linear regression analyses to predict FMS severity measured by FIQ from depression (PHQ-9), anxiety (GAD-7) and bipolar disorder determined by MDQ, psychiatric diagnosis or both. Depression and anxiety but not a positive screen for BD either by MDQ , prior clinical diagnosis of BD or either, remained independent predictors of FIQ variance.
Conclusion: The utility of MDQ as a screening tool for BD in patients with FMS, as well as the impact of a psychiatric diagnosis of BD on FMS measures and severity, needs to be further evaluated. Nevertheless, patients with high MDQ scores seem to have more severe depressive and anxiety symptoms and score higher on FMS measures of severity and impact.
To cite this abstract in AMA style:
Gota C, Kaouk S, Yaseen K, Jhala N, Wilke W. Utility of Mood Disorders Questionnaire in Fibromyalgia: Data from the Cleveland Clinic Fibromyalgia Registry [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/utility-of-mood-disorders-questionnaire-in-fibromyalgia-data-from-the-cleveland-clinic-fibromyalgia-registry/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/utility-of-mood-disorders-questionnaire-in-fibromyalgia-data-from-the-cleveland-clinic-fibromyalgia-registry/