Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Antiphospholipid syndrome (APS) is characterized by thromboembolic and obstetric morbidity associated with antiphospholipid antibodies (aPL) in systemic lupus erythematosus (SLE). This study aims to evaluate the prevalence of aPL profile, and identify clinical and genetic risk factors associated with thrombotic and obstetric events in Korean patients with SLE.
Methods: Patients with SLE were enrolled and followed from 1998 to 2018 in Hanyang BAE lupus cohort and were investigated clinical and aPL profile [lupus anticoagulant (LAC), anticardiolipin antibodies (aCL), and anti-β2-glycoprotein1 antibodies (aβ2-GP1)]. We genotyped SLE patients using genome-wide association study (GWAS) array (Affymetrix Axiom-KOR, 833K SNPs). To determine risk factors for APS, clinical and genetic variables were analyzed by logistic regression.
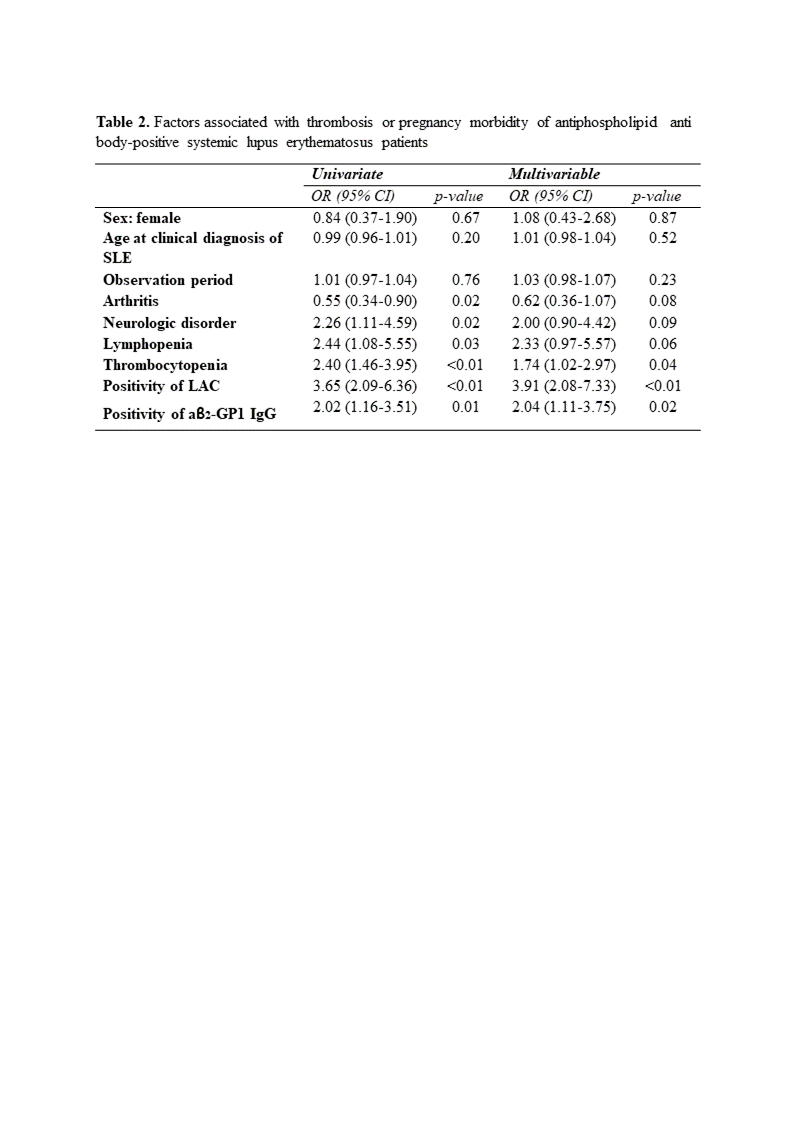
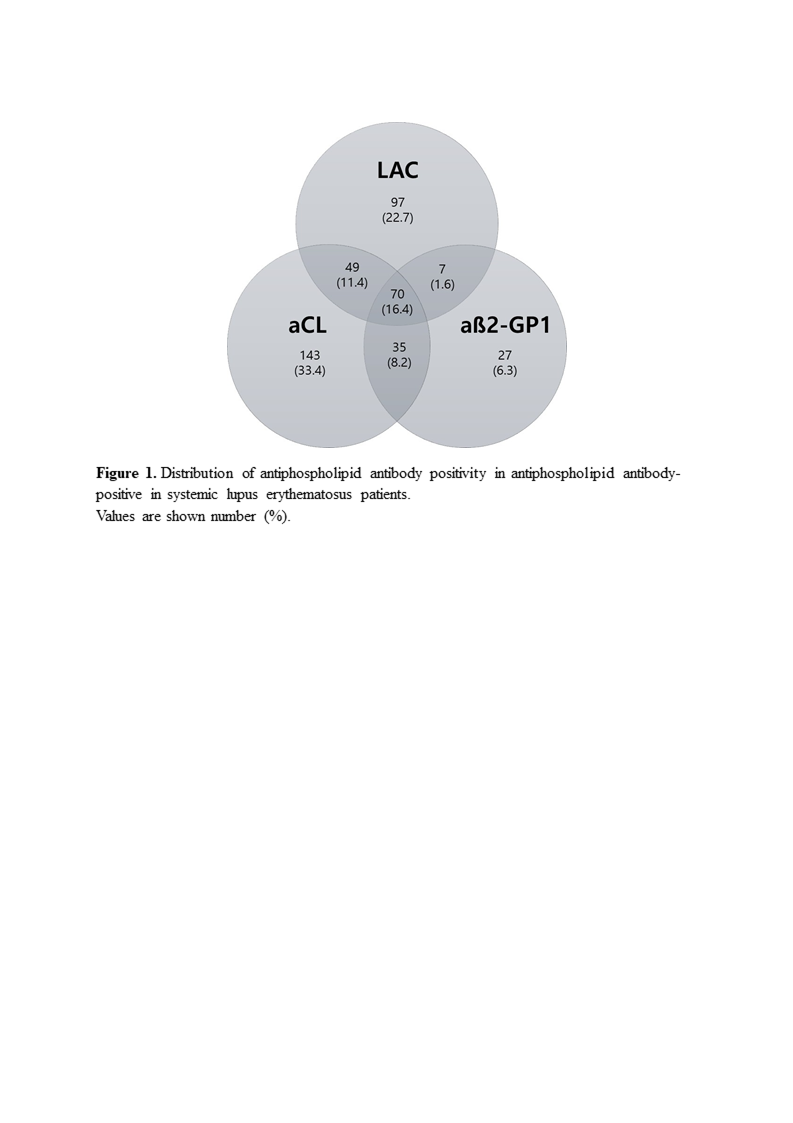
Results: Among 1,167 SLE patients, 428 (36.7%) had at least one aPL (aPL(+)). In patients with aPL(+) SLE, the number of patients with LAC, aCL and aβ2-GP1 was 223 (52.1%), 297 (69.4%), and 139 (32.5%), respectively. Triple aPL positivity was observed in 70 (16.4%). Among 428 aPL(+) SLE patients, 79 (18.5%) had thrombosis or pregnancy morbidity as clinical criteria of APS, and 42 (9.8%) were satisfied with classification criteria of APS. When comparing the groups with and without thrombosis or pregnancy morbidity in aPL(+) SLE patients, multivariable regression analysis indicated that thrombocytopenia (p=0.04), positivity of LAC (p< 0.01), and positivity of aβ2-GP1 IgG (p=0.02) were associated with the occurrence of thrombosis or pregnancy morbidity in aPL(+) SLE. We identified eight SNPs were associated with development of aPL in SLE patients (p< 5×10-5). We also identified that two genes have significant effects on thrombosis manifestations in aPL(+) SLE patients (p< 5×10-6). Among them, top gene showed the high risk association with APS(+) SLE (odds ratio=6.2) that influenced on regulation of Wnt pathway and vascular permeability.
Conclusion: In this study, 36.7% of Korean SLE patients showed aPL positivity. Eight SNPs were associated with the development of aPL in SLE, two genes with thrombosis manifestations in aPL(+) SLE, and the top gene with APS(+) SLE. As clinical factors, thrombocytopenia, positivity of LAC, and positivity of aβ2-GP1 IgG were significantly associated with the occurrence of APS related thrombosis or pregnancy morbidity in aPL(+) SLE. These results may help clinicians to better risk stratify aPL(+) SLE patients.
To cite this abstract in AMA style:
Kim J, Ahn G, Choi J, Lee J, Park Y, Bang S, Bae S. Clinical and Genetic Factors Associated with Thrombosis or Pregnancy Morbidity of Antiphospholipid Antibody-Positive Systemic Lupus Erythematosus Patients [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/clinical-and-genetic-factors-associated-with-thrombosis-or-pregnancy-morbidity-of-antiphospholipid-antibody-positive-systemic-lupus-erythematosus-patients/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-and-genetic-factors-associated-with-thrombosis-or-pregnancy-morbidity-of-antiphospholipid-antibody-positive-systemic-lupus-erythematosus-patients/