Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Recurrent thrombosis is an uncommon complication of patients with antiphospholipid syndrome (APS), usually related with persistent high levels of antiphospholipid antibodies (aPL), specially classic aPL (anticardiolipin antibodies, aCL or lupus anticoagulant, LA). The role of other aPL, including anti-phosphatidylserine/prothrombin (PS/PT) antibodies, anti B2 glycoprotein 1 (B2GP1) and anti domain 1 against B2GP1 as markers of recurrence in APS, it is less well known. Our aim was to determinate the relationship between the presence of different aPL (criteria and non-criteria aPL) with recurrent thrombosis in a cohort of patients with APS, including patients with primary APS and secondary APS (related with SLE)
Methods: We conducted a prospective single center study including patients with diagnosis of APS (Sidney criteria). A wide panel of aPL antibodies were measured at the moment of study inclusion, then, a prospective follow up was made according daily clinical practice. New thrombotic and non-thrombotic manifestations were recorded during follow-up. Anti-D1 B2GPI antibodies were tested using a chemiluminescent immunoassay (QUANTA Flash, Inova Diagnostics). In addition, anti PS/PT (IgG and IgM), aCL (IgG and IgM) and anti B2GP1 (IgG and IgM) were measured at baseline by ELISA. LA was detected according to International guidelines.
Baseline patient characteristics were summarized using counts and percentages or median and for categorical and continuous variables. Comparison across groups was done using Chi-squared, Fisher’s Exact, or Mann–Whitney tests as appropriate. Kaplan–Meier for time to event analysis was used to determine risk factors for thrombotic events during follow-up.
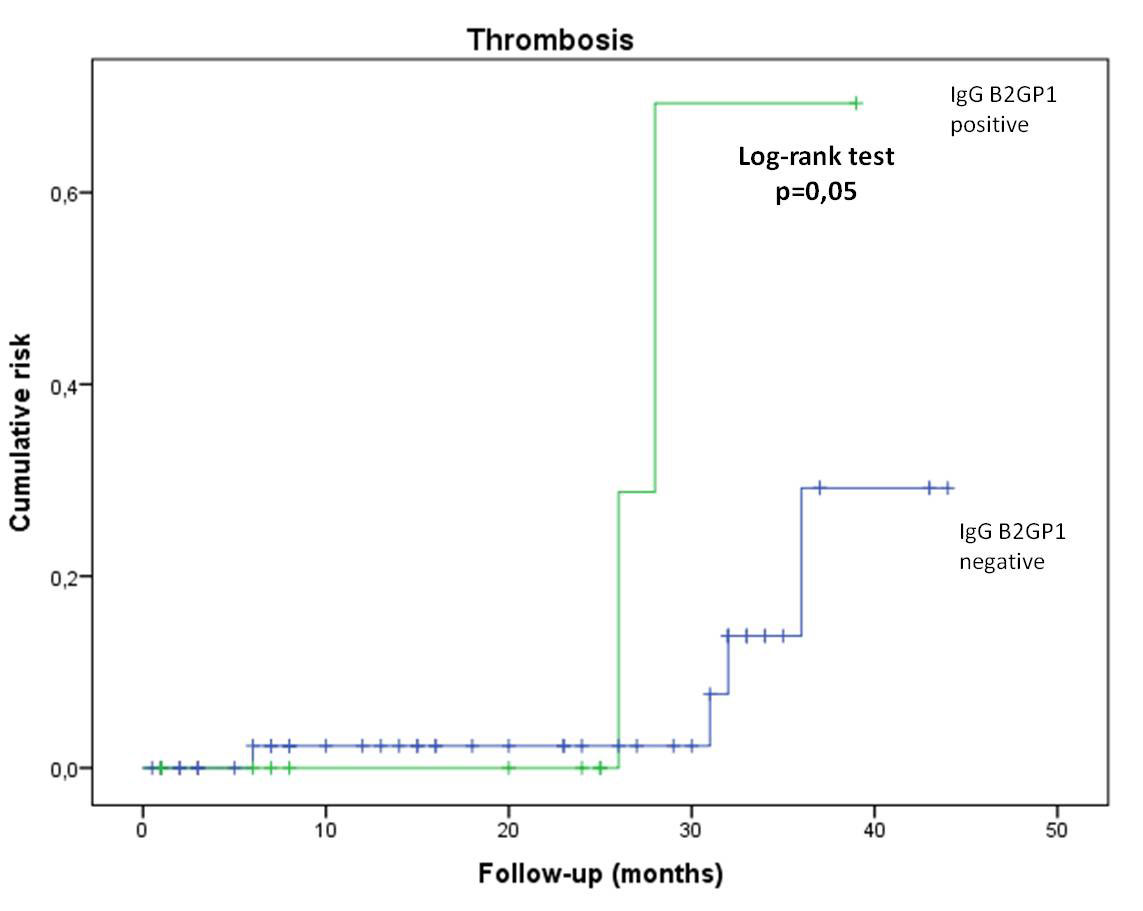
Results: One hundred and sixty eight patients were included, 87% of patients were female with a mean age of 34.0 ± 12.8 years. aPL profile was done in 145 patients with secondary APS and 23 patients primary APS. Clinical follow-up was available in 91 patients. Mean follow-up was 20.6 ± 13.8 months (range 1-46 months). New thrombotic episodes occurred in 8 out of 91 (8.8%) of patients (6 DVT and 2 arterial), 5 of them despite anticoagulation therapy (4 vitamin K antagonist and 1 Dabigatran).We also documented 6 new episodes of thrombocytopenia and 2 new fetal losses. Overall, anti IgG B2GP1 antibodies were related with recurrent thrombosis (28 vs 7%, p=0,022), arterial thrombosis (6.7 vs 0%, p=0,05) and LA with recurrent thrombocytopenia (12,9 vs 0%, p=0,049). In survival analysis, IgG B2GP1 were related with a significant cumulative risk of thrombosis (Figure). No relationship between non-criteria aPL or triple positivity was found with recurrence. No clinically relevant major or minor bleeding occurred
Conclusion: In our cohort of patients with APS, IgG B2GP1 antibodies were related with recurrent thrombotic events. Given the low rate of new events, a longer follow-up is needed to establish further relationships.
To cite this abstract in AMA style:
Urrego T, Frade-Sosa B, Hernández A, Ruiz S, Rua C, Duque J, Vanegas-García A, Muñoz-Vahos C, González L, Vasquez G, Gómez-Puerta J. Relationship Between Recurrent Thrombosis and the Antiphospholipid Antibodies Profile in a Cohort of Patients with Antiphospholipid Syndrome [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/relationship-between-recurrent-thrombosis-and-the-antiphospholipid-antibodies-profile-in-a-cohort-of-patients-with-antiphospholipid-syndrome/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/relationship-between-recurrent-thrombosis-and-the-antiphospholipid-antibodies-profile-in-a-cohort-of-patients-with-antiphospholipid-syndrome/