Session Information
Date: Wednesday, October 24, 2018
Title: 6W008 ACR Abstract: Pediatric Rheum–Clinical III: Assessment Tools & Biomarkers (2916–2921)
Session Type: ACR Concurrent Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose:
There is growing awareness of severe and often fatal chronic lung disease in patients with systemic juvenile idiopathic arthritis (sJIA). However, clinical features and risk factors for sJIA- associated lung disease are poorly characterized.
Objectives:
1- Describe clinical characteristics and immunological findings in patients with sJIA- associated lung disease.
2- Determine risk factors and predictors of lung disease in sJIA patients.
Methods:
This study was approved by CCHMC Institutional Review Board, and informed consent was obtained from all patients. Clinical data was abstracted from medical records. We matched 12 sJIA patients with chronic with lung disease to 24 controls without lung disease using current age and gender (1:2) in a case-control design. We used Fischer exact and T.test for comparisons.
Results:
Since 2010, we evaluated 12 patients (including second opinion) with sJIA-associated lung disease. Nearly half (5/12) were evaluated over the last year. In the last 5 years 74 patients with sJIA have had their primary rheumatology care at CCHMC. Of those patients, 6 developed lung disease, indicating both increased detection and an incidence as high as 8%.
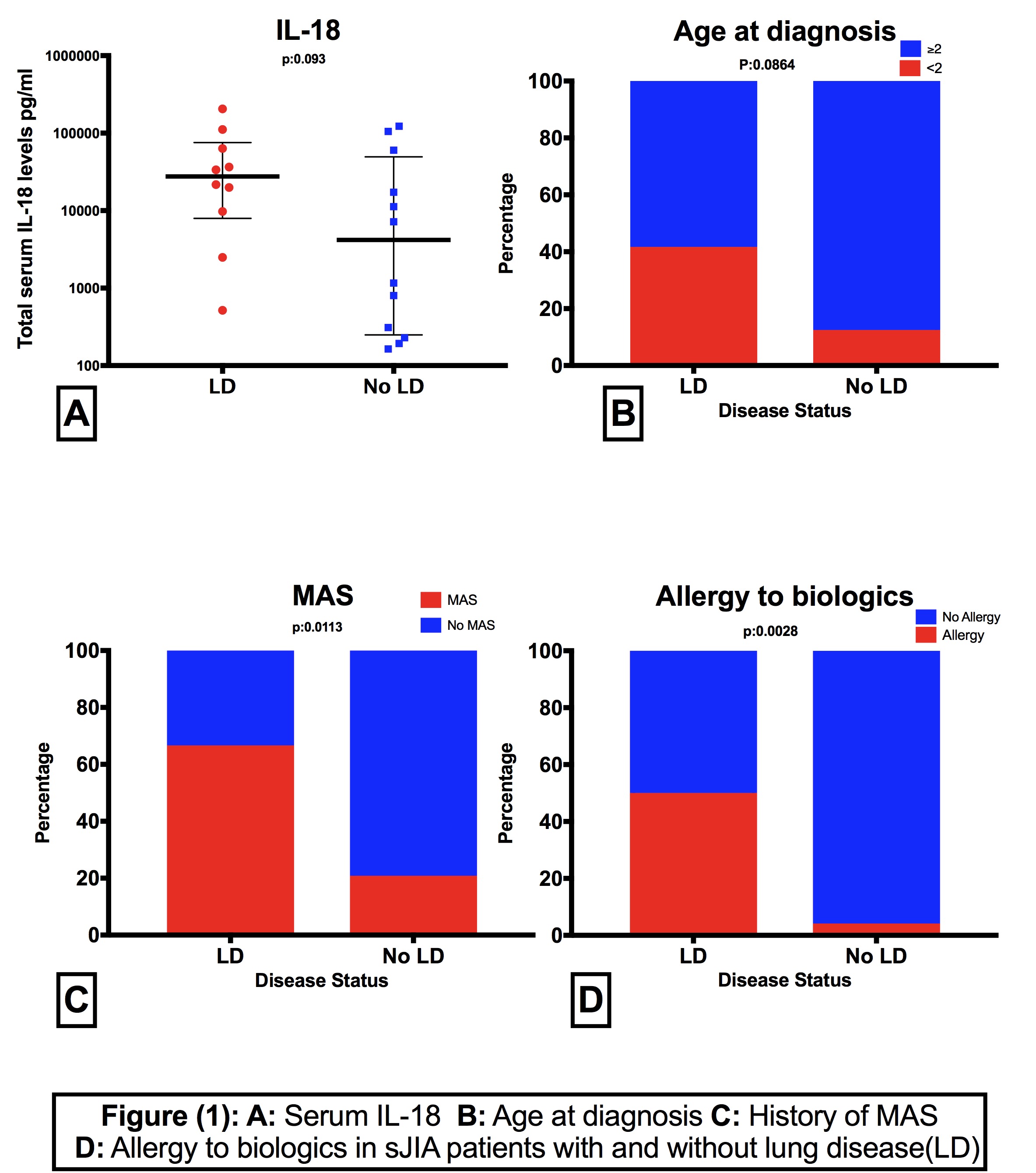
In our cohort, 83% of patients with lung disease (10/12) were diagnosed with sJIA before age 5 (42% before age 2). Median age at diagnosis was 2.5 years (IQR: 0.75-4.25). When compared to controls, lung disease patients were diagnosed with sJIA at younger age, many before age 2 (OR: 5, p=0.08) (Figure 1-B). In the majority (75%) lung disease symptoms started within 1 year of diagnosis with mean time from sJIA onset to lung disease diagnosis of (1.65 ± 1.26).
Interestingly, all patients with lung disease presented with prominent systemic features and two-thirds (66.6%) have history of macrophage activation syndrome (MAS). Compared to controls, lung disease patients were significantly more likely to have had MAS with OR of 7.6 (p=0.0113) (Figure 1-C). They also had markedly elevated IL-18 levels (Median 27,612.0, IQR: 9746-63,417). IL-18 levels were higher than those in patients with active sJIA without lung disease (Median 7194 IQR: 907-60,260 (p:0.032)), but when compared to age-matched controls it did not achieve significance (P:0.093) (Figure1-A).
Moreover, significantly more patients with lung disease (6 patients) developed allergic/anaphylactic reaction to one of the cytokine-targeted biologics (mostly tocilizumab) with an OR of 23 (p:0.0028) (Figure 1-D).
Conclusion:
Severe lung disease is increasingly recognized in children with sJIA, particularly in those presenting at younger age, with prominent systemic features, history of MAS, or allergy to biologics. These patients also tend to have ongoing chronic inflammation with highly elevated IL-18 levels. Early screening and expedited work up of this fatal complication is prudent especially in patients with beforementioned risk factors.
To cite this abstract in AMA style:
Yasin S, Towe C, Fall N, Grom A, Schulert G. An Epidemic: Severe Lung Disease in Patients with Systemic Juvenile Idiopathic Arthritis, Risk Factors and Predictors [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/an-epidemic-severe-lung-disease-in-patients-with-systemic-juvenile-idiopathic-arthritis-risk-factors-and-predictors/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/an-epidemic-severe-lung-disease-in-patients-with-systemic-juvenile-idiopathic-arthritis-risk-factors-and-predictors/