Session Information
Date: Tuesday, October 23, 2018
Title: 5T091 ACR Abstract: Spondyloarthritis Incl PsA–Clinical IV: Comorbid/Related Conditions(2826–2831)
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose:
Systemic inflammation contributes to the excess risk of cardiovascular disease (CVD) in PsA. We had demonstrated that achieving sustained minimal disease activity (sMDA) was associated with protective effect on subclinical atherosclerosis and arterial stiffness1. Yet, it is unclear if remission or stable low disease activity over time is sufficient to diminish the CV harmful effects of systemic inflammation.
Methods:
We conducted a post hoc analysis of the PsA MDA vascular study1. 101 PsA patients without overt CVD were recruited in this 2-year prospective study. All patients received protocolized treatment aiming at MDA. High-resolution ultrasound for subclinical atherosclerosis and arterial stiffness were assessed annually. Carotid plaque progression was defined as increased number or region harboring plaque. 4 definitions of remission/inactive disease were used: MDA and very low disease activity (VLDA)2 defined as 5 & 7 MDA cut points are met. Disease Activity Index for Psoriatic Arthritis remission (DAPSA-rem) and low disease activity (DAPSA-LDA) were defined as DAPSA≤4 and ≤14. Sustained disease control was defined as achieving these targets at each consecutive visit from month 12 till month 24.
Results:
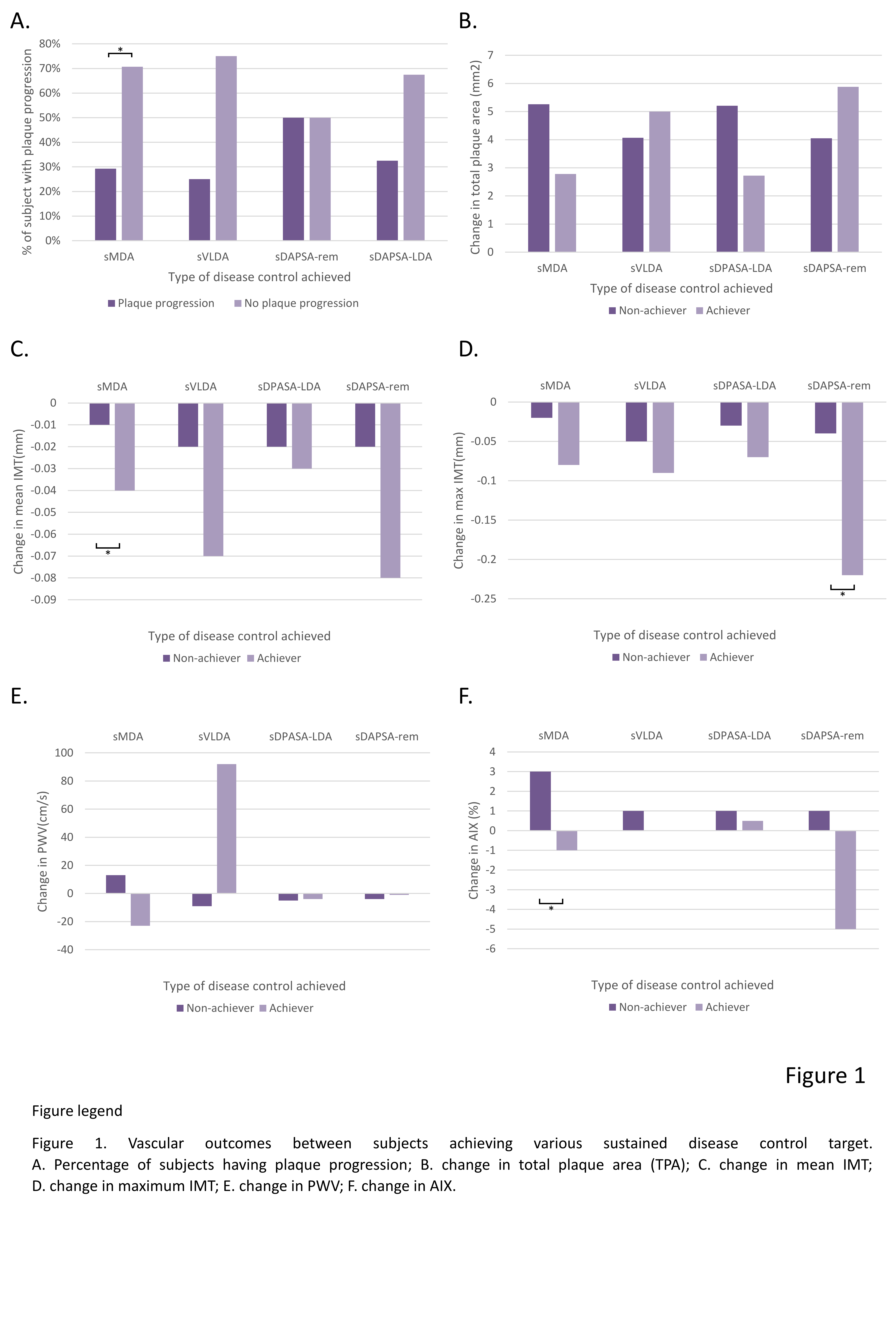
90 PsA patients [male: 52 (58%); age: 50±11] who completed follow up were included in this analysis. Significant improvement in disease activity was observed (MDA: 15 [17%] at baseline vs 62 [69%] at 2-year, p<0.001; DAPSA 19 [13,32] at baseline: vs 7 [4,14] at 2 year, p<0.001). 46%, 4%, 44% and 4% of subjects achieved sMDA) sustained VLDA (sVLDA), sustained DAPSA-LDA and sustained DAPSA-rem respectively. 34 (38%) had plaque progression. The rate of plaque progression was significantly lower in sMDA group when compared to those who did not. Achieving sMDA was also associated with less progression in mean intima-media thickness (IMT) and augmentation index (AIx) (Fig 1). Using multivariate analysis, achieving sMDA had protective effect on plaque progression, less increase in total plaque area (TPA), mean IMT and AIX after adjusting baseline covariates (Table 1). No significant association between progression of vascular parameters and other treatment targets was observed.
Conclusion:
Achievement of sMDA was associated with protective effect in subclinical atherosclerosis and arterial stiffness progression but not sDAPSA-LDA. Multidimensional domain of disease control is preferable for minimizing CV risk in PsA.
|
Table 1 – Multivariate analysis on the change in mean/max IMT, AIX, PWV, any plaque progression and change TPA |
|||
|
|
Multi-variate analysis |
||
|
OR |
95%CI |
p-value |
|
|
Plaque progression 1 |
|||
|
Age |
1.069 |
1.009 to 1.131 |
0.023 |
|
Physicians’ global assessment, baseline |
0.964 |
0.936 to 0.993 |
0.016 |
|
Plasma LDL-C, baseline |
2.628 |
1.310 to 5.493 |
0.007 |
|
bDMARDs use at baseline |
0.110 |
0.018 to 0.652 |
0.015 |
|
Achieved sustained MDA |
0.273 |
0.088 to 0.846 |
0.024 |
|
Multi-variate analysis |
|||
|
β |
95%CI |
p-value |
|
|
Change in total plaque area2 |
|||
|
BMI, kg/m2, baseline |
-0.428 |
-0.760 to -0.096 |
0.012 |
|
Plasma LDL-C, baseline |
2.828 |
0.723 to 4.932 |
0.009 |
|
Achieved sustained MDA |
-3.919 |
-7.181 to -0.657 |
0.019 |
|
Change in mean IMT3 |
|||
|
bDMARDs use throughout the year |
-0.034 |
-0.065 to -0.004 |
0.028 |
|
Achieved sustained MDA |
-0.037 |
-0.066 to -0.007 |
0.014 |
|
Change in max IMT4 |
|||
|
Age |
0.003 |
0.000 to 0.005 |
0.038 |
|
CRP, baseline |
0.002 |
0.000 to 0.005 |
0.036 |
|
NSAIDs use, baseline |
0.122 |
0.045 to 0.199 |
0.003 |
|
Maximum IMT, baseline |
-0.455 |
-0.646 to -0.264 |
<0.001 |
|
Change in PWV5 |
|||
|
Age |
4.953 |
0.919 to 8.986 |
0.017 |
|
PWV, baseline |
-0.483 |
-0.676 to -0.289 |
<0.001 |
|
Achieved sustained MDA |
-71.4 |
-143.2 to 0.2 |
0.051 |
|
Change in AIX6 |
|||
|
Male gender |
3.332 |
0.105 to 6.560 |
0.043 |
|
Achieved sustained MDA |
-3.059 |
-6.067 to -0.051 |
0.046 |
|
1Adjusted for age, gender, baseline deformed joint count, physicians’ global assessment score, plasma total triglyceride, total cholesterol, LDL-C, use of bDMARDs and presence of carotid plaque at baseline; 2Adjusted for age, gender, baseline BMI, VAS pain score, patient’s global assessment score, plasma total triglyceride, total cholesterol, LDL-C level and use of csDMARDs; 3Adjusted for disease duration, baseline CRP, Framingham risk score, use of NSAIDs and use of bDMARDs throughout the year; 4 Adjusted age, gender, baseline CRP, waist-to-hip ratio, plasma total cholesterol, LDL-C level, NSAIDs use and maximum IMT; 5 Adjusted for age, gender, baseline abdominal obesity and PWV; 6 adjusted with age, gender, baseline AIX and csDMARDs use throughout the year; IMT-intima media thickness; AIX-augmentation index; PWV-pulse wave velocity; TPA-total plaque area; LDL-C- low density lipoprotein cholesterol; BMI-body mass index; csDMARDs- conventional synthetic disease modifying anti-rheumatic drugs; bDMARDs-biologic disease modifying anti-rheumatic drugs; VAS-visual analogue scale; CRP-C-reactive protein; NSAIDs-non-steroidal anti-inflammatory drugs Reference: 1. Isaac T et al, Can achieving sustained Minimal Disease Activity (MDA) prevent progression of subclinical atherosclerosis? A two-year prospective cohort study in Psoriatic Arthritis. 19th Asia Pacific League of Associations for Rheumatology Congress (APLAR); Dubai: International Journal of Rheumatic Diseases; 2017 2. Coates LC et al, Defining minimal disease activity in psoriatic arthritis: a proposed objective target for treatment. Ann Rheum Dis. 2010;69:48-53.
|
|||
To cite this abstract in AMA style:
Cheng IT, Shang Q, Li EKM, Wong P, Tam LHP, Zhu TY, Chang MM, LEE JJ, Lee PA, Tam LS. Remission Targets and Prevention of Subclinical Atherosclerosis in Psoriatic Arthritis- Which Target Should We Choose? [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/remission-targets-and-prevention-of-subclinical-atherosclerosis-in-psoriatic-arthritis-which-target-should-we-choose/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/remission-targets-and-prevention-of-subclinical-atherosclerosis-in-psoriatic-arthritis-which-target-should-we-choose/