Session Information
Date: Tuesday, October 23, 2018
Title: Vasculitis Poster III: Immunosuppressive Therapy in Giant Cell Arteritis and Polymyalgia Rheumatica
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
Giant Cell Arteritis (GCA) is the most common systemic vasculitis in patient over 50 years of age. It is a medical emergency as it may lead to ischemic complications, including permanent visual loss in 20 % of untreated patients. Early diagnosis enabling a rapid initiation of treatment is of critical importance. Positive Temporal Artery Biopsy (TAB) is still the gold standard test. However, a negative TAB does not rule out the disease. Encephalic high-field MRI, temporal arteries ultrasonography (US) or fluorescein and indocyanine green angiogram (FA) have been widely studied as diagnostic tests. However, there is currently no consensus nor clearly identified algorithm for their use in a current practice, either alone or in combination.
Our objective was to develop a new multimodal imaging algorithm based on a combination of encephalic high-field (3T) MRI, ultrasonography (US) and retinal angiogram (fluorescein (FA) and indocyanine green (ICGA)) , to improve the diagnosis of GCA
Methods:
All patients referred for suspected GCA at our center from December 2014 to October 2017 were prospectively included in this study. The study was approved by an official external Ethical Review Board. PatientÕs informed consent was obtained upon inclusion.
For each patient, encephalic 3T MRI, cervical and temporal arteries US and retinal angiogram (RA) were performed. Subsequently, a TAB was performed.
TAB-positive patients were considered cases of GCA ; TAB-negative patients files were reviewed by two experts in internal medicine to determine whether they were or not cases of GCA based on ACR criteria.
Diagnostic accuracy of the combination of MRI, US and RAwas statistically evaluated, first separately for each imaging modality, then using a multimodal classification tree.
Results:
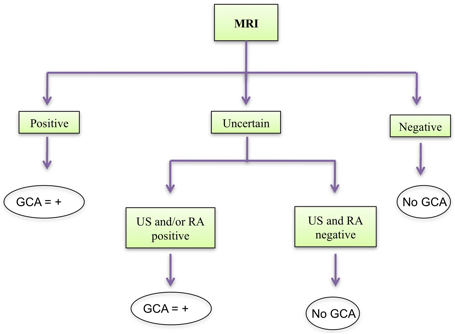
Forty five patients were included. GCA was diagnosed in 25 patients, TAB was positive in 19 patients. Thirty one patients presented a partial vision loss. MRI was positive in 24/44 patients, negative in 16/44 patients and uncertain in 4/44 cases. No patients with negative MRI had GCA. When MRI was positive, 23/24 patients had GCA. If MRI was uncertain and both US and RA were negative, final diagnosis was no GCA ; if either US and/or RA was positive, final diagnosis was GCA. We propose the following algorithm, with a positive predictive value of 96.2 % and a negative predictive value of 100%.
Conclusion:
We propose an algorithm that is highly predictive for GCA diagnosis and can be a valuable tool in suspected cases of GCA.
When GCA is suspected, we suggest to perform 3T encephalic MRI first and if uncertain, to add US and RA.
To cite this abstract in AMA style:
Lecler A, Sené T, Picard H, Leturcq T, Zuber K, Charbonneau F, Vignal-Clermont C, Clavel G. Multi Modal Imaging Algorithm to Improve the Accuracy for the Diagnosis of Giant Cell Arteritis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/multi-modal-imaging-algorithm-to-improve-the-accuracy-for-the-diagnosis-of-giant-cell-arteritis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/multi-modal-imaging-algorithm-to-improve-the-accuracy-for-the-diagnosis-of-giant-cell-arteritis/